- Graduate School
- CHARLOTTESVILLE, VA
- Rating 4.86 out of 5 7 reviews

Doctoral programs
All doctoral programs offered, nursing science, education, and practice, similar grad schools, explore programs at similar grad schools.
- Virginia Commonwealth University
- RICHMOND, VA
- Johns Hopkins University
- BALTIMORE, MD
- Rating 4.44 out of 5 32 reviews
- Georgetown University
- NW WASHINGTON, DC
- Rating 4 out of 5 1 review
- University of Pennsylvania
- PHILADELPHIA, PA
- Rating 5 out of 5 5 reviews
The University of Virginia
Search form, you are here.
- Graduate Admission

Thomas Jefferson believed that learning was a lifelong pursuit. From the arts and sciences to law and business, UVA offers some of the nation’s premier graduate programs.
The School of Nursing is a community of scholars having as its central purpose the enrichment of the human mind. Within this community, the Doctor of Philosophy in Nursing Program seeks to prepare scholars who will advance nursing knowledge. Scholarly achievement in nursing is accomplished in a spirit of free inquiry directed toward a better understanding of human existence, especially in relation to health and illness. Nurse scholars must participate in the study of particular phenomena and in the identification of central domains related to these phenomena. This requires that students be well informed about advanced practice in professional nursing.
Nursing knowledge is advanced through association with other disciplines and is often enhanced by the work of other university scholars. Central to the education of nurse scholars is the opportunity to interact with other scholars throughout the university community. Through dialogue and study with these professionals, nurse scholars expand their understanding of health and illness and the biological, environmental, sociocultural, ethical, legal, philosophic, and historic factors influencing nursing care.
Scholars must be inquisitive, informed, and committed. This requires expertise in the principles and methods of inquiry and an informed imagination for exploring substantive areas in nursing. The ultimate goal of this inquiry is to enhance nursing’s contribution to the health of all persons.
Purpose and Program Aims
The major purpose of the doctoral program in nursing is to prepare scholars with expertise in selected substantive areas who will contribute to nursing theory and practice through systematic inquiry. Aims of the doctoral program in nursing are to prepare scholars who will:
- Demonstrate advanced knowledge of nursing, related sciences and humanities, and methods of inquiry.
- Expand the research base of nursing theory and practice.
- Serve the Commonwealth, the nation, and the world by addressing major nursing and health care issues in a scholarly manner.
Program Components
The PhD program consists of courses, research and teaching activities, and required experiential elements (comprehensive exam, grant submission, dissertation proposal defense, dissertation and its defense). We support our PhD students in obtaining the skills needed for teaching in a future faculty role. Many students gain teaching experience within a funded Graduate Teaching Assistantship. Students are encouraged to work with their advisors to identify other teaching resources within the University as well.
Nursing Field
The evolution and current state of nursing knowledge are examined from both historical and philosophical perspectives and serve as the basis for the establishment of critical inquiry and study in addressing the increasingly complex health care needs of vulnerable populations.
The research component of the program includes courses in research design and methodology, statistics, individually designed research practicums, and the dissertation. The dissertation is a culminating experience which requires the student to plan and implement a research study of significance to nursing.
Students planning to use qualitative research methods should take a second advanced qualitative methods course, and students planning to use quantitative research methods should take an additional advanced quantitative methods course that is specific to the method they plan to use for their dissertation research.
Cognate Minor (9-12 credits)
The cognate requirement includes course work in a single cognate field or combination of fields outside the School of Nursing. The cognate field is intended to complement the student’s major scholarly focus. Cognates must be at the 5000 level or higher and be offered from departments outside of the School of Nursing (not GNUR classes).
Electives (3-6 credits)
Electives are selected by the student on the basis of individual interest. These should complement the total program of study and may be taken both within and outside the School of Nursing. Electives must be at the 5000 level or higher and may include GNUR classes.
NOTE: Students must have a total of 15 credit hours of cognates plus electives. If 12 credit hours of cognates, 3 credit hours of electives are required. If 9 credit hours of cognates, 6 credit hours of electives are required. All cognate and elective credits must be graded on an A through F scale.
Comprehensive Exam
All students are required to write a comprehensive exam. The comprehensive examination may occur within the last semester of course work, but must be held no later than: (1) if coursework is completed in the spring or summer, comprehensive exams must be completed by the end of the following fall semester; (2) if coursework is completed in the fall semester, comprehensive exam must be completed before the start of the following fall semester. Students may apply to the Director of the PhD Program for an extension of one semester maximum. Failure to complete the examination within the allotted timeframe constitutes a failure to make satisfactory progression and can be grounds for involuntary withdrawal from the program. Students can apply to take comprehensive exams after completion of course work requirements as represented in the Plan of Study, and comprehensive exams must be completed prior to the defense of the dissertation proposal. The purpose of the examination is to demonstrate the student’s ability to synthesize knowledge in the student’s area of expertise, to visualize the long-term development of a program of research in that area, and to place the planned dissertation research in the context of that program of research and the area of knowledge (more details in the School of Nursing PhD Handbook).
Once the Comprehensive exam is completed, students must enroll in GNUR 9890, Dissertation Seminar, every semester until graduation unless exempted by dissertation advisor.
Dissertation (12 credits of GNUR 9999)
The dissertation is a culminating experience which requires the student to plan and implement a research study of significance to nursing.
Application for Degrees
PhD degrees are granted in December, May, and August. The student must be registered for the fall semester to receive the degree in December, for the spring semester to receive the degree in May, and for summer session to receive the degree in August. The student must apply to graduate via the Student Information System (SIS).
Voluntary Withdrawal
A graduate student may not voluntarily withdraw from the Graduate School of Arts and Sciences later than one week immediately preceding the beginning of course examinations. An official application to withdraw must be obtained from the Office of the Dean of the Graduate School of Arts and Sciences and must be approved in writing by the dean, with a statement of the reason for the withdrawal. The student must report to the Office of the Dean of Students for an exit interview. All student identification cards are to be deposited with the Office of the Dean of Students at the time of withdrawal. The official withdrawal form is forwarded to the University Registrar, who notifies all other administrative offices of the withdrawal action.
A student who withdraws from the University for reasons of ill health must notify the Department of Student Health, and subsequent medical clearance from Student Health is among the requirements for readmission. Failure to comply with the above regulations subjects the student to suspension from the University by the vice president for student affairs.
Readmission After Voluntary Withdrawal
Readmission to the Graduate School of Arts and Sciences is not automatic; after an absence of a semester or longer, a former student must apply for readmission to the Graduate School. To apply for readmission to the University, the student must submit an application per the requirements of the Graduate School of Arts and Sciences.
Enforced Withdrawal
The student may be required to withdraw from the University if the advisor, the dissertation chair, the responsible department members, and the dean of the Graduate School of Arts and Sciences determine that the student is making unsatisfactory progress toward a degree.
Program Description
Required courses.
(32-33 credits)
- HHE 7650 - Ethics & Law of Human Subject Research Credits: 2
- BIMS 7100 - Research Ethics Credits: 1
- GNUR 8435 - Scholarship in Research Ethics Credits: 1
- GNUR 8130 - Statistical Methods for Health Care Research I Credits: 3
- GNUR 8140 - Statistical Methods for Health Care Research II Credits: 3
- GNUR 8110 - Quantitative Research Methods Credits: 3
- GNUR 8120 - Introduction to Qualitative Research Methods Credits: 3
- GNUR 8210 - Scholarly Writing for Nursing Science Credits: 3
- GNUR 8220 - Philosophy of Science and Development of Nursing Knowledge Credits: 3
- GNUR 8230 - Historical Inquiry in Nursing Credits: 3
- GNUR 8410 - Grant Writing Credits: 3
- GNUR 9110 - Research Practicum I Credits: 1 to 4
4 credit hours total of GNUR 9110, Research Practicum, are required
- GNUR 9890 - Dissertation Seminar Credits: 1
(9-12 credits) Requirement includes course work in a single field or combination of fields outside of nursing that complement the student’s major scholarly focus. Cognates plus electives must total at least 15 credits.
(3-6 credits) Electives are selected on the basis of individual interest and should complement the total program of study. Cognates plus electives must total at least 15 credits.
Dissertation
(12 credits) Dissertation is a culminating experience that requires the student to plan and implement a research study of significance to nursing.
Programs are individualized to meet degree requirements.

Home / Nursing Degree / Best Ph.D. in Nursing Programs – 2024
Best Ph.D. in Nursing Programs – 2024
2024 - Best Ph.D. in Nursing Programs
Which ph.d. in nursing program is right for me, on-campus vs. online phd in nursing programs, admission requirements & curriculum, which nursing careers require a ph.d., list of ph.d. in nursing programs.

Many nurses, after working at the bedside, seek different ways to utilize their knowledge and clinical skills. Some prefer to advance their career and become nurse practitioners and earn either an MSN or DNP . However, some nurses hope to take their knowledge and apply it to something a bit different than a clinical focus – research and education. Ph.D. prepared nursing helps address critical issues in healthcare and even helps shape policies and legislation.
Nursing knowledge in healthcare and research is essential. Nurses provide a unique perspective and use a patient-centered approach to various issues in healthcare. This perspective helps to benefit both patients and organizations and improves care outcomes. Since many who choose the Ph.D. in a nursing pathway do so to become educators, this degree type paves the way to shape the next generation of nurses.
Already have a nursing degree and looking to advance your education to a Ph.D. in Nursing? Bridge programs such as the BSN to Ph.D. , MSN to Ph.D. , and DNP to Ph.D . are available.

For highly skilled and ambitious nurses, the Ph.D. in Nursing pathway is the pinnacle of registered nursing education. Many RNs feel called to research and academia, and a Ph.D. can provide ample opportunities for success in these areas. There are few things more important than choosing the right Ph.D. program, which is why we have ranked the top online/hybrid Ph.D. in Nursing programs available across the country. Check out our rankings below and take the first step toward a high-level nursing career.
For more information on our top nursing school rankings, visit our Methodology Page ( https://www.registerednursing.org/rankings-methodology/ ).
Texas Woman's University
At Texas Woman's University in Houston, Ph.D. students become experts in nursing theory development and research methods as they embark on a journey to bolster the future of nursing. Many graduates of the Doctor of Philosophy in Nursing program go on to teach at the college level while others pursue a career in nursing administration or research.
- PhD in Nursing Science Online/Hybrid
- DNP to PhD Bridge Program Online/Hybrid

Recipient of Quality Matters Implementation Plan award. Offering hybrid or online-only degree completion options. The historical women’s college does admit men.
Endicott College
Through research, innovation, and collaboration, the Doctor of Philosophy in Nursing degree at Endicott College enables nurses to become leaders both in and outside the world of academia. The hybrid program offers flexible weekend and evening in-person and online course delivery options.
- Ph.D. in Nursing Online/Hybrid

- A private college located outside of Boston.
- Includes a loan option for those looking to teach.
- Very low faculty-to-student ratios for each cohort.
Mercer University
Nurses can transition their bedside and clinical experiences into scholarship when they decide to earn their Ph.D. at Mercer University. The online terminal degree readies nurses for careers in education and research to advance the profession of nursing.
- Doctor of Philosophy (Ph.D.) in Nursing Online/Hybrid

- A dissertation is required to complete the degree.
- The program receives funding via the Nurse Faculty Loan Program.
- A private research university in Macon, Georgia.
University of Central Florida
Nurses can perform different professional roles aside from caring for patients in a hospital or clinical setting. From conducting original research to teaching, nurses can pursue their Ph.D. in Nursing online at the University of Central Florida. Students learn to contribute to the discipline as an academic.
- PhD in Nursing: BSN to PhD Online/Hybrid
- PhD in Nursing: MSN to PhD Online/Hybrid

• Only open to RNs licensed in Florida. • Students complete Dissertation / Doctoral Research. • One of the first universities to offer a nursing Ph.D.
William Carey University
William Carey University offers a Doctor of Philosophy in Nursing Education Program (DNP to PhD). Nurses who think they’d like to make a career educating the next generation of healthcare professionals can enroll in this online program. Nurses can continue to work while earning this terminal degree.
- Nursing Education - DNP to PhD Online/Hybrid

- Can be completed in 2-3 years.
- There are four weekend meetings per year (two synchronous online and two in-person)
- A private Christian university located in Hattiesburg, MS.
Selecting a Ph.D. program can be challenging. Each nurse has individual work and family demands, so the school needs to fit into the nurse’s busy life. There are a few considerations nurses should take into account when looking for a Ph.D. program:
- Online Learning vs. Classroom Learning – Selecting an online program vs. an on-campus program is a personal choice. While some prefer the convenience and flexibility of online learning, some enjoy face-to-face, interactive learning, along with peer support. Some programs are 100% online, and some require minimal campus visits (often referred to as "hybrid" programs). Whichever the learning method, nurses should choose the one right for them.
- Accreditation – National accreditation is critical when selecting a Ph.D. program. Proper accreditation ensures the school meets strict quality standards and allows the nurse to pursue future degree options. Also, nursing boards in some states require national (as opposed to local) accreditation for licensure. Students should look for accreditation by the Commission on Collegiate Nursing Education ( CCNE ) or the Accreditation Commission for Education in Nursing ( ACEN ) when researching schools.
- Program History – Some nursing programs, including online programs, are popping up left and right. Students should be cautious and do their research when looking at Ph.D. programs. Schools that have been around a long time tend to be more reputable, and they also likely have enough data (for example, graduation rates) that the student can use to measure the program’s success.
- Program Cost – Cost is a significant factor when deciding to return to school. Most websites are transparent with the tuition cost and associated expenses, so there won't be any surprises. Many schools offer financial aid options as well as the choice to attend part-time. However, students should also prepare for additional expenses such as immunization requirements, technology equipment requirements, supplies, parking fees, and graduation or university fees.
- Residency/Internship Requirements – Studying course material is one part of Ph.D. programs, but nurses must also apply what they’ve learned to real life. Nurses should make sure that whichever program they choose, they are able to meet the practicum requirements. Ensuring they have resources and mentors in the community and surrounding organizations is crucial to the student's success.
RELATED : Dual DNP/PhD Programs
As stated earlier, choosing an online program vs. an on-campus depends on the needs of the student. Below are some advantages of both online and on-campus programs:
Online Ph.D. Nursing Program Advantages
- Flexible schedule – Nurses can work around the clock. They may work weekends, holidays, swing shifts, and graveyard shifts. For this reason, a school must be flexible. Online programs allow nurses to study course material when they can as well as learn at their own pace. They can submit assignments and correspond with instructors and peers electronically, not having to wait until the class or the instructor's office hours.
- Tuition and Costs – An advantage of online Ph.D. programs is cost. In some cases, students may select a school that is based outside their state. Schools sometimes don't charge different tuition rates for out-of-state students in their online programs, which is a significant cost-saver and allows more education options. Students are encouraged to research this thoroughly, however.
- Accessibility and Convenience – As stated earlier, online programs are far more flexible than campus programs. At the touch of a button, students can access learning materials, peers, instructors, and online learning modules. They can study in the middle of the night, on holidays, on weekends, or whenever it's convenient. They are not limited to certain hours on certain days. Plus, they don’t need to waste time commuting, parking, and walking to class.
- Fast Completion – Many online programs boast rapid completion. While students need to be wary of schools that advertise this (specific curricula must be completed), some legitimate online programs do allow students to finish faster than traditional, campus programs. This is because students can study at their own pace. If eager to start out in their new role, online learning might be the way to go.
On-Campus Ph.D. in Nursing Program Advantages
While more and more online nursing programs are popping up, some students still prefer traditional campus learning. Some advantages of on-campus education include:
- The ability to interact face-to-face with peers and instructors
- Not having to worry about technology issues
- Not needing to spend extra money on electronic or technological supplies
- Accreditation is usually not a concern
While admission requirements for a Ph.D. in nursing program may vary between schools, prospective students may be required to:
- Hold a current, unencumbered RN/APRN license
- Hold a BSN or MSN from an accredited university (some schools allow admission for BSN nurses)
- Have completed a specific number of clinical hours
- Provide transcripts from all schools attended
- Have a GPA of 3.5 or higher (specific GPA requirements may vary between schools)
- Submit a written goal statement to include research career goals
- Interview with faculty
Ph.D. in Nursing Course Topics
Since the Ph.D. in nursing is more research and education-focused, the course topics differ from that of a more clinically-focused degree program (such as the DNP). Course topics may include:
- Qualitative and quantitative research
- Scientific inquiry
- Synthesis and application of nursing knowledge
- Research development
- Chronic illness and care systems
Program Length
The didactic/clinical portion of the Ph.D. program can take around 1-3 years to complete depending on if the nurse starts from a BSN or MSN. The first year is reserved for core courses, while the following year and beyond focus on electives specific to the student's goals and the completion of a teaching practicum. Students are also required to complete a dissertation as well; the dissertation period may take another 1-3 years to complete, depending on the student’s area of focus.
While some nurses choose to earn a Ph.D. to fulfill their educational goals, sometimes it is a requirement for certain positions. Examples include:
- Nurse educator or instructor
- Nurse or hospital administrator
- Research facilities
- Government and public health nursing roles
Some may even consider a Post-Doctoral Nursing Fellowship Program .
Popular with nurses interested in teaching and research, Ph.D. nursing programs have grown in popularity and are available at schools across the United States. Below you will find a state-by-state guide on available Ph.D. in nursing programs.
Jump to Your State Listings
University of alabama at birmingham.
- Doctor of Philosophy in Nursing Campus
Arizona State University
- Nursing and Healthcare Innovation, PhD Campus
University of Arizona
- Nursing (PHD) Online
University of Arkansas for Medical Sciences (UAMS)
- PhD in Nursing Campus
Azusa Pacific University Monrovia
- Nursing, PhD Campus
Loma Linda University
- BS to PhD in Nursing Online
- MS to PhD in Nursing Online
- Nursing Science and Health-Care Leadership Doctor of Philosophy Campus
- UCLA School of Nursing Doctor of Philosophy (PhD) Campus
University of California San Francisco
- PhD, Nursing Campus
- PhD in Nursing: Health Policy Campus
University of California, Irvine
University of san diego.
- Doctor of Philosophy in Nursing- BSN to PhD Campus
- Doctor of Philosophy in Nursing- Post-MSN PhD Campus
- Doctor of Philosophy in Nursing- DNP to PhD Campus
University of Colorado Anschutz Medical Campus
- Doctor of Philosophy (PhD) in Nursing Hybrid
University of Northern Colorado
- Nursing Education PhD Online
Connecticut
University of connecticut.
- School of Nursing - PhD Program Campus
Yale University
- PhD Program in Nursing Campus
University of Delaware
- Doctor of Philosophy (PhD) in Nursing Science Campus
Barry University
- Doctor of Philosophy in Nursing
Florida Atlantic University
- PhD in Nursing Program Campus
- PhD in Nursing Program BSN to PhD Campus
- PhD in Nursing Program MSN to PhD Campus
- PhD in Nursing Program DNP to PhD Campus
Florida International University
- BSN-to-PhD in Nursing Campus
- PhD in Nursing: BSN to PhD Online
- PhD in Nursing: MSN to PhD Online
University of Florida
- PhD in Nursing Sciences Campus
- PhD in Nursing Sciences: BSN to PhD Campus
- Adult Gerontology NP: MSN to PhD Campus
University of Miami
- Doctor of Philosophy (PhD) in Nursing Campus
University of South Florida
- PhD Program in Nursing Science Campus
Augusta University
- Doctor of Philosophy with a Major in Nursing Hybrid
Emory University
- Doctor of Philosophy in Nursing Hybrid
Georgia State University
- Doctor Of Philosophy In Nursing Hybrid
- Doctor of Philosophy (Ph.D.) in Nursing Online
University of Hawai'i at Manoa
- PhD in Nursing Online
Idaho State University
Illinois state university.
- PhD in Nursing Hybrid
Loyola University of Chicago
Rush university.
- Nursing Science (PhD) Online
University of Illinois at Chicago (UIC)
- Doctor of Philosophy Campus
Indiana University Online
- PhD in Nursing Science Online
Purdue University
- PhD in Nursing* Campus
University of Iowa
- College of Nursing PhD Campus
- College of Nursing PhD BSN to PhD Campus
- College of Nursing PhD MSN to PhD Campus
University of Kansas
University of louisville, southern university and a&m college.
- Doctor of Philosophy in Nursing (PhD) Campus
Johns Hopkins University
University of maryland.
- Post-BSN to PhD in Nursing (without a master's) Campus
- Post-BSN with a Master's to PhD in Nursing Campus
- Post-Master's to PhD in Nursing Campus
Massachusetts
Boston college.
- Ph.D. in Nursing Hybrid
Northeastern University
- PhD in Nursing
University of Massachusetts Amherst
- Nursing PhD Campus
University of Massachusetts Boston
University of massachusetts lowell.
- Ph.D. in Nursing with Health Promotion focus Hybrid
University of Massachusetts Medical School
Michigan state university.
- Ph.D. in Nursing Campus
Oakland University
- Ph.D. in Nursing
University of Michigan
- Nursing, Ph.D. Campus

Wayne State University
- Ph.D. in Nursing Online
University of Minnesota
Mississippi, university of mississippi medical center.
- Nursing Education - DNP to PhD Online
Barnes-Jewish College Goldfarb School of Nursing
- Doctor of Philosophy in Nursing (PhD) Hybrid
Mizzou Online- University of Missouri
- Nursing: Online doctorate Online
University Of Missouri Kansas City
- Nursing PhD Hybrid
University of Missouri - St. Louis
- Nursing PhD Online
University of Missouri Health
- Interdisciplinary Nursing PhD Campus
University of Nebraska Medical Center
University of nevada, las vegas.
- Doctor of Philosophy in Nursing; Nursing Education Online
- Doctor of Philosophy in Nursing; Post Doctor of Nursing Practice Online
- Doctor of Philosophy - Interdisciplinary Health Sciences Campus
Rutgers School of Nursing
Seton hall university, the university of new mexico, adelphi university, binghamton university, columbia university, nyu rory meyers college of nursing, pace university - pleasantville campus.
- Doctor Of Philosophy In Nursing, Phd Campus
Stony Brook University
University at buffalo.
- Doctor of Philosophy (PhD) in Nursing Online
North Carolina
Duke university.
- PhD Program in Nursing Online
East Carolina University
The university of north carolina at chapel hill, the university of north carolina at greensboro, north dakota, university of north dakota, case western reserve university.
- Dual Doctorate PhD/DNP Hybrid
Kent State University
The ohio state university.
- Post-Master's PhD in Nursing Campus
- BSN to PhD in Nursing Campus
University of Cincinnati
- PhD in Nursing Research Campus
Oklahoma City University
- BSN-PhD in Nursing Campus
The University of Oklahoma
Oregon health & sciences university, pennsylvania, drexel university.
- Nursing: MSN-PhD Joint Degree Program Campus
University of Pennsylvania School of Nursing
- Doctor of Philosophy in Nursing (MSN-PhD) Campus
University of Pittsburgh
Rhode island, university of rhode island, south carolina, medical university of south carolina.
- Ph.D. in Nursing Science Online
University of South Carolina
- Doctor of Philosophy in Nursing Science (Ph.D.) Campus
East Tennessee State University
- College of Nursing - PhD Program Hybrid
The University of Tennessee Health Science Center- Memphis
- DNP/PhD Dual Degree Campus
The University of Tennessee, Knoxville
- Doctor of Philosophy in Nursing (PhD) BSN to PhD Campus
- Doctor of Philosophy in Nursing (PhD) MSN to PhD Campus
University of Memphis
- Doctor of Philosophy in Nursing (PhD) Online
- DNP to PhD Bridge Program Online
The University of Texas Medical Branch at Galveston
- Nursing PhD BSN to PhD Online
- Nursing PhD MSN to PhD Online
The University of Texas at Arlington
The university of texas at austin.
- Alternate Entry Doctoral (AE-PhD) in Nursing Campus
- Doctoral (PhD) in Nursing Campus
The University of Texas at Tyler
University of texas health science center at san antonio - ut health san antonio.
- BSN to PhD FT in Nursing Campus
- BSN to PhD PT in Nursing Campus
- Post-MSN FT in Nursing Campus
- Post-MSN PhD PT in Nursing Campus
University of Texas School of Nursing at Houston
University of utah, george mason university.
- Nursing, PhD Hybrid
Hampton University
- Nursing, PhD Online
University of Virginia
Virginia commonwealth university.
- Online Nursing PHD Online
University of Washington
- PhD Doctor of Philosophy in Nursing Science Campus
Washington State University Vancouver
West virginia, west virginia university, marquette university.
- Ph.D. In Nursing Campus
University of Wisconsin-Madison
University of wisconsin-milwaukee.
- Nursing BS to PhD Campus
- Nursing Online PhD Online
Are we missing your school's program or need to update information listed? Please contact us so we can make the necessary changes.
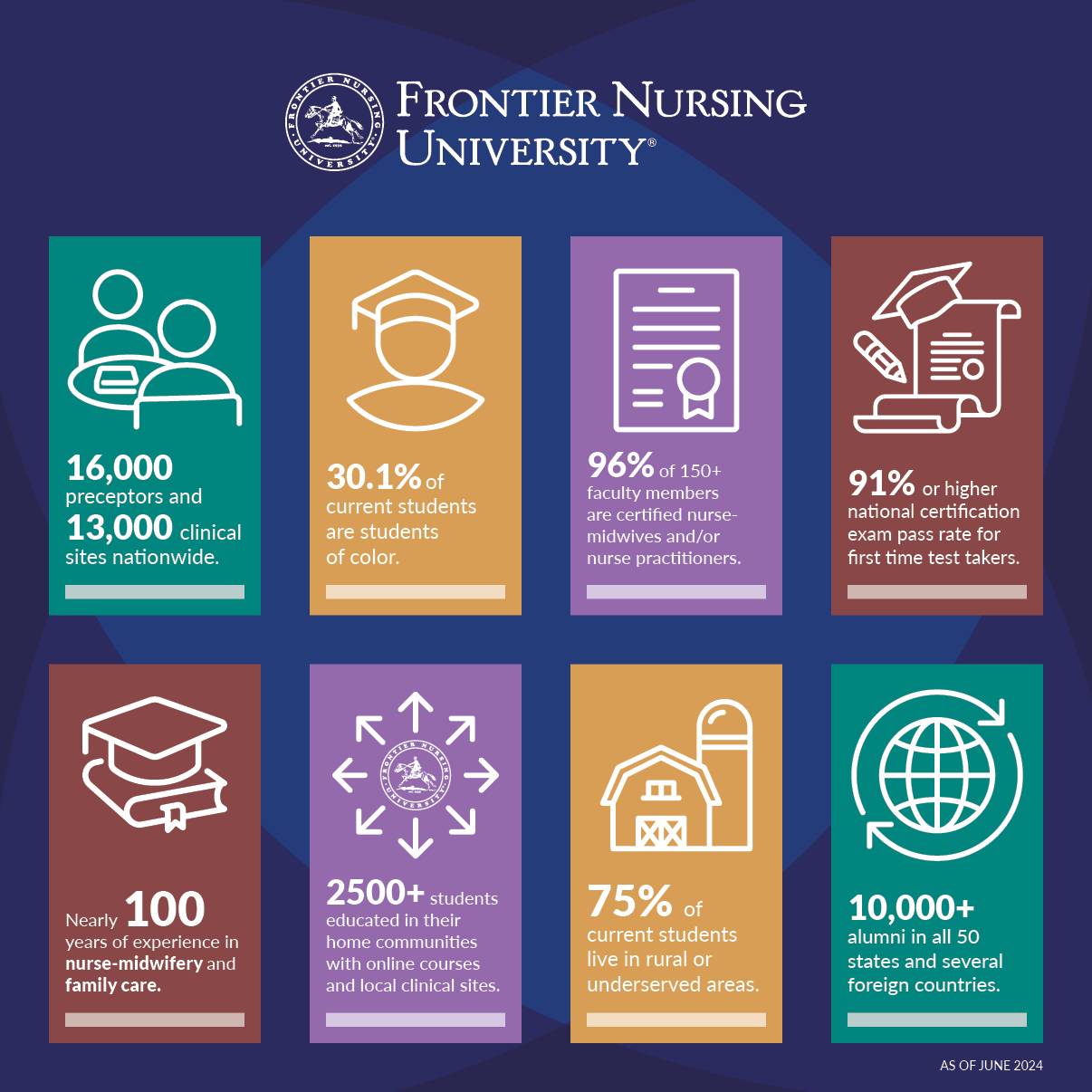
Frontier Nursing University
Distance Education from the Birthplace of Nurse-Midwifery and Family Nursing in America

Diversity, Equity, and Inclusion
FNU has been nationally recognized for preparing graduate nursing and midwifery students to meet the healthcare demands of an increasingly diverse patient population.
Culture Of Caring
FNU fosters a Culture of Caring built on five main elements: Professionalism, Inclusivity, Respect, Positive Communication and Mutual Support.
Our Mission
Our mission is to educate compassionate leaders in primary care to serve all individuals with an emphasis on diverse, rural, and underserved populations.
Clinical Placement Services
At FNU, you are not alone in your search for clinical site placement. We are with you every step of the way.

Questions? Visit our Admissions FAQ
Application Deadlines
Why Choose Frontier Nursing University?

Choose the path that best fits your goals.

Doctor of Nursing Practice

Master of Science in Nursing

Post-Graduate Certificate
Discover your passion.
Frontier Nursing University programs are designed for compassionate nurses committed to caring for women and families. If you aren’t sure where to start, let us help you find the best program for you. FIND YOUR PATH
Mark Your Calendar
Spring term 2025 application deadline, summer term 2025 application deadline, fall term 2025 application deadline.
- Google Calendar
- Outlook 365
- Outlook Live
- Export .ics file
- Export Outlook .ics file
Review Visit by ACME
Frontier Nursing University wishes to announce that we will host a site visit for the continuation of its Post-Graduate Certificate program and Master’s program by the Accreditation Commission for Midwifery Education (ACME). You are invited to meet with the site visit team and share your comments about the program in person at a meeting scheduled for November 13-15. LEARN MORE
FNU is recognized as a Great College to Work For for the fourth year in a row. The Great Colleges to Work For program is one of the largest and most respected workplace-recognition programs in the country. FNU is a great place to work because of the outstanding people who are fully committed to our students and our mission.
FNU Information
Request Information
Frontier Nursing University has been approved to participate in the National Council for State Authorization Reciprocity Agreements.
Privacy Statement
2050 Lexington Road Versailles, KY 40383 (859) 251-4700
For education verification requests: • Web: degreeverify.org • Mail: National Student Clearinghouse, 2300 Dulles Station Boulevard, Suite 220, Herndon, VA 20171
For program inquiries: [email protected] or 859-279-0890
Accreditation
Learn more about FNU's Accreditation
View FNU Policies & Procedures

Melanie A. Mariano, MSN, FNP-BC (she/her) is interested in advancing health equity by identifying and rectifying systemic racism in clinical decision-making and expanding community health services. She is a BSN and MSN graduate of the University of Pennsylvania’s School of Nursing. Upon graduation from Penn Nursing, she worked to establish a nursing presence at the Free Library of Philadelphia to connect marginalized populations to health services. Clinically, she currently works as a family nurse practitioner in the Atlanta Metro area. She is currently completing her work toward both a Doctor of Nursing Practice and Master of Public Health degrees at Johns Hopkins University School of Nursing and Bloomberg School of Public Health.

Kathleen Scott earned her bachelor’s degree of Science in Nursing in 2006 from Hawaii Pacific University, Her Master’s Degree of Science in Nursing in 2008 from Frontier University and her Doctor of Nursing Practice in 2019 from Frontier University. She became an ACNM Fellow in 2024. She practices at Nebraska Medicine as a Certified Nurse Midwife and is a volunteer faculty member at University of Nebraska. In 2023, Dr. Scott’s innovative approach to teaching earned her the Excellence in Educational Service award through the University of Nebraska. Throughout her education, she was mentored and encouraged by her professors and colleagues. This support and inspiration greatly affected her success and allowed for additional educational opportunities that have motivated her to continue to learn well after her formal education had ended. She is committed to improving perinatal health outcomes within her community to decrease the maternal morbidity and mortality rates with her involvement in local nonprofit groups. The results of her DNP project, a project focused on identifying and treating anxiety and depression antenatally, influenced, and improved care provided to patients. She cofounded a volunteer doula program using allied health students to provide bedside support for long term antepartum and intrapartum patients. She works with local doula organizations, improving their continued educational opportunities and fostering cohesive integration into the birth team. Throughout her career she has taught a multitude of students and residents, nurturing a commitment to evidence based and compassionate care.

She is a member of several professional organizations, including the American Academy of Nurse Practitioners, the California Association for Nurse Practitioners, and Sigma Theta Tau International Honor Society in Nursing.Discover Midwives.

Dr. Robert White is the recipient of a Mentored Research Training Grant (MRTG) from the Foundation for Anesthesia Education and Research (FAER) for his project titled “Health Disparities in Obstetrical Care and Delivery Outcomes Before and After Implementation of an Enhanced Recovery After Surgery Protocol.”
Obstetrical healthcare disparities have been extensively reported, with Black women experiencing disproportionate mortality and severe maternal morbidity, explained Dr. White. The two-year, $250,000 grant will support Dr. White’s research into the effect of implementing Enhanced Recovery After Surgery (ERAS) protocols on delivery outcomes, and the development of a data-driven dashboard for clinicians. The support will further Dr. White’s research into interventions that promote patient equality and equity. Dr. Kane Pryor is the primary faculty mentor.
In the first phase of the project, Dr. White and researchers from the Center for Perioperative Outcomes will investigate obstetrical healthcare disparities on a national scale using databases from the Healthcare Cost and Utilization Project (HCUP). In the second phase, they will study the impact of the evidence-based ERAS protocols.
“We’re looking at pre- and post-implementation of ERAS protocols in terms of outcomes for white, Black, Hispanic and Asian patients to see if these new care processes attenuate or eliminate disparities that exist,” said Dr. White.
Dr. White’s goal is to apply the research from the first two research questions to the development of a data-driven dashboard for clinicians that will help provide patient care recommendations and data visualizations.
“Maternal mortality and morbidity is a major crisis afflicting our nation,” said Dr. White. “It’s exciting that healthcare disparities projects are getting an increased level of funding and that solutions to these national crises are being investigated.”
Dr. Robert White is an assistant professor of anesthesiology and was a Van Poznak Research Scholar in the Department of Anesthesiology. He obtained his undergraduate degree from Cornell University, his medical degree and a master’s in clinical research from Albert Einstein College of Medicine, and completed his anesthesia residency and obstetric anesthesia fellowship training at NewYork-Presbyterian/Weill Cornell Medical Center. He has authored numerous manuscripts exploring healthcare disparities in perioperative outcomes and quality of care.
The FAER MRTG grant provides support for early-career training of anesthesiologist-scientists to achieve independence as scientific investigators.

Robert M. (Bob) Silver, MD has been in the division of maternal fetal medicine at the University of Utah Health Sciences Center for over 30 years. He holds the John A. Dixon Presidential Endowed Chair and is Professor and Chairman of the department of Obstetrics and Gynecology. Dr. Silver’s clinical and research interests include recurrent pregnancy loss and stillbirth, cesarean delivery, placenta accreta spectrum, preeclampsia, vaginal birth after cesarean delivery, immunologic diseases in pregnancy, and medical disorders in pregnancy.

Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
With over 15 years of experience in public health and nursing, Nikia has dedicated herself to advancing reproductive rights and justice, birth justice, and midwifery. Her passion for midwifery shines through in her commitment to diversifying the workforce of midwives and birth workers, especially in the southern United States. As a fervent disruptor of the current healthcare system, Nikia is pioneering new models of care that prioritize midwifery and center the needs of Black and brown communities. Every day, she works Tirelessly to ensure that all individuals have the agency and resources to make informed decisions about their sexual and reproductive health.
At CHOICES Center for Reproductive Health, Nikia serves as the Chief Clinical Officer, spearheading interfaces that have led to the establishment of the first nonprofit comprehensive reproductive health care center, the first Black midwifery fellowship program and the city’s inaugural birth center. Beyond her clinical leadership, Nikia sits on the Board of Directors for both the American College of Nurse Midwives and SisterReach, Tennessee’s foremost Reproductive Justice organization.
Driven by a profound sense of purpose, Nikia Grayson is transforming the landscape of reproductive healthcare, leaving an indelible mark on the lives of those she serves and the communities she uplifts.

Michelle Debbink, MD/PhD FACOG is an Assistant Professor of Maternal-Fetal Medicine at the University of Utah in Salt Lake City. She grew up in the Air Force and enjoyed moving frequently around the US and abroad. She received her bachelor’s degree in Sociology and Policy Studies from Rice University, and her MD and PhD in Health Services Organization and Policy (social epidemiology focus) at the University of Michigan in Ann Arbor. She completed her obstetrics and gynecology residency at University of Michigan as well, and then moved to the University of Utah for her Maternal-Fetal Medicine Fellowship. She is a current Reproductive Scientist Development Program scholar, and is funded to conduct research on the community and geographic drivers of racial and ethnic inequities in severe maternal morbidity and maternal mortality. In particular, her research focuses on a population health-community engaged translational continuum to amplify resilience and build interventions to close gaps in perinatal care in partnership with American Indian/Alaska Native and Native Hawaiian/Pacific Islander women and birthing people. She also serves as the Departmental Vice Chair for Equity, Diversity, and Inclusion for the ObGyn Department at the University of Utah, and the Assistant Program Director for the Women’s Health Equity Fellowship at the University of Utah.

Holly Powell Kennedy, PhD, CNM, FACNM, FAAN was the inaugural Helen Varney Professor of Midwifery (now emeritus) at the Yale University School of Nursing. She has served as the President of the American College of Nurse-Midwives and received the 2016 Hattie Hemschemeyer Award, their highest honor. Her program of research is focused on a greater understanding of the effectiveness and outcomes of specific models of care during the childbearing year, especially is support of childbearing physiology. She was a Fulbright Distinguished Fellowship at King’s College London in 2008 and is currently a Fulbright Specialist. She is a retired Colonel in the US Army Nurse Corps Reserve.

Karlie Porter Masaga is a Certified Nurse Midwife and Womens Health Nurse Practitioner providing care to women across their lifespan. Karlie started her career as a Midwife and Nurse Practitioner in Utah County. She has since joined the Birthcare Healthcare team and is enjoying her time caring for women in the Salt Lake and surrounding areas. Karlie is passionate about providing evidence-based care to women. She strives to ensure all her patients feel heard, understood, and receive best practice at each stage of their life from teenage years, through childbearing, labor, birth, and menopause.
Karlie is an adjunct faculty for University of Utah College of Nursing teaching new midwifery and women’s health providers. She has a strong passion for helping those who come from different backgrounds and cultures. Prior to going into the medical field, Karlie worked for the State of Utah Juvenile Justice system where her love for teens from diverse backgrounds flourished. During her Doctorate of Nursing Practice degree at University of Utah Karlie took part in the research of sexually transmitted infections in Fiji with the University of California San Francisco. Karlie has continued to stay connected with Pacific Islanders through her church, community and family. She is currently working on outreach to Native Hawaiian and Pacific Islander women who are seeking healthcare by providing services at South Main Clinic. During her time off you will find her paddle boarding, biking, playing sports, and enjoying a lot of laughter with her husband and family.

Jeelan Fall is a Certified Nurse Midwife and Women’s Health Nurse Practitioner providing full scope services including routine gynecologic care throughout the lifespan, contraception, pre-conception counseling, pregnancy, labor, birth, and postpartum care. Jeelan is a first-generation graduate with a life-long calling to the world of childbirth and women’s health. She believes in the philosophy of shared decision-making between patients and their care providers. She received a Bachelor of Science in Nursing from Westminster College in Salt Lake City, Utah, and a Doctor of Nursing Practice from the University of Utah.
Dr Fall has a particular passion for maternal health disparities and how they tie into increased rates of morbidity and mortality among mothers and neonates who are Black, Indigenous, and People of Color (BIPOC). In her free time, she enjoys traveling to any place in the world with a beach and spending time with her family.

Eugene Declercq, Ph.D., M.B.A., is a professor of community health sciences at the Boston University School of Public Health and professor on the faculty of Obstetrics and Gynecology at the Boston University School of Medicine. His current research focuses primarily on maternal mortality and morbidity. He is part of the team that has produced six reports on women’s experiences in childbirth, Listening to Mothers. He is a current member of the Massachusetts Maternal Mortality Review Committee and on the board of March for Moms. He was principal investigator on two NIH funded collaborative projects examining child and maternal outcomes associated with Assisted Reproductive Technologies (MOSART project) and is one of the founders of the Pregnancy to Early Life Longitudinal (PELL) data system that has linked vital statistics, hospital, and administrative data on more than 1,200,000 births in Massachusetts since 1998. He has also been active in a variety of public health projects in his hometown of Lawrence, Massachusetts.
He is the founder of the website www.birthbythenumbers.org, where additional data on maternal mortality and other maternal and infant health outcomes can be found. He is also a recipient of the Martha May Eliot Award from the American Public Health Association for service to maternal and child health and the Greg Alexander Award for research in maternal and child health epidemiology.
He has Ph.D. and M.S. degrees from Florida State University and a M.BA. from University of Massachusetts at Amherst.

Dr. Yvonne T. Maddox, Ph.D. is President and Chief Executive Officer of the TA Thornton Foundation, a family foundation dedicated to promoting the health and wellness of underserved communities. Dr. Maddox previously served as Vice President for Research and Professor of Allied Health Sciences at the Uniformed Services University of the Health Sciences (USUHS), a part of the Department of Defense, where she oversaw a robust clinical and basic science research portfolio, including infectious diseases, trauma and critical care medicine, health maintenance, post-traumatic stress, and traumatic brain injury. Prior to joining USUHS, Dr. Maddox held many leadership positions at the National Institutes of Health (NIH), including Acting Director of the National Institute on Minority Health and Health Disparities, Deputy Director of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, and Acting Deputy Director of the entire NIH.
Throughout her academic and government career, Dr. Maddox has been a champion of issues related to women, children, and underserved populations. Among her many accomplishments include leading teams of international scientists in the field of reproductive health as part of bi-lateral agreements between the U.S., India, and Africa; directing the highly recognized NIH program (the Back to Sleep Campaign) to reduce sudden infant death syndrome (SIDS); creating the NIH Down Syndrome (DS) Consortium, a federal/private partnership to advance research in DS; and initiating the NIH-funded Well Prepared and Fit for Life childhood obesity reduction programs. Dr. Maddox has numerous research and public policy publications and is a recognized speaker in the area of public trust and community engagement in medical research. Her memberships on critically important committees and working groups, several as chairperson, demonstrate her commitment to improving the health and wellness of minority populations and to increasing their opportunities in science and biomedical research. She currently serves as the Senior Strategic Advisor for the NIH Path to Excellence and Innovation Initiative to advance funding opportunities for Historical Black Colleges and Universities.
Among her memberships on advisory boards and committees include: the National Institute for Environmental Health Sciences (NIEHS)/NIH Council Working Group on Equity, Diversity, and Inclusion; Nutrition Research Advisory Group, Friedman School of Nutrition, Science and Policy, Tufts University; Advisory Council, Food is Medicine Institute, Tufts University; the American Society for Nutrition Foundation Board of Trustees Executive Committee; the Black AIDS Institute Scientific Advisory Committee, and the Miraki Innovation Board of Directors.
Dr. Maddox has received many honors and awards, including the United States Presidential Distinguished Executive Rank Award (the highest honor for a career civil servant), United States Presidential Meritorious Rank Award, U.S. Department of Health and Human Services (DHHS) Career Achievement Award, Public Health Service Special Recognition Award, DHHS Secretary’s Award, NIH Director’s Award (including one that bears her name), National Down Syndrome Society Champion of Change Award, Research Down Syndrome Foundation Light the Way Award, Delta Sigma Theta Award for Public Service, the National Council of Negro Women Partnership Award, the Hela Leadership Award for Excellence in Reproductive Medicine, Induction into the Historical Black Colleges and Universities (HBCUs) Hall of Fame, and selection as one of the top 30 Women in Higher Education by the Journal, Diverse: Issues in Higher Education. She is the recipient of several honorary degrees.
Dr. Maddox received her B.S. in biology from Virginia Union University, Richmond, and her Ph.D. in physiology from Georgetown University. She studied as a Visiting Scientist at the French Atomic Energy Commission, Saclay, France and graduated from the Senior Managers in Government Program of the Kennedy School of Government, Harvard University.

Wendy Post is a seasoned nursing professional and a passionate advocate for maternal health with over 25 years of experience. She holds a Doctor of Nursing Practice (DNP) and is currently pursuing a PhD at George Washington University School of Nursing. Her extensive career in nursing has been dedicated to addressing maternal morbidity and mortality, particularly in underserved communities impacted by maternal health deserts and maternal morbidity and mortality.
In addition to her academic pursuits, Wendy has taken on the role of a forensic nurse examiner in Maryland, enhancing her ability to support populations impacted by trauma. She is the founder of “The Birth Mark,” an organization committed to improving maternal health outcomes globally. Her organization has a specific branch dedicated to supporting women affected by maternal mortality, reflecting her deep commitment to advocacy and support for bereaved families.
Wendy’s current research involves a pilot study that explores the experiences of eyewitnesses and medical examiners involved in maternal deaths. This study employs verbal and social autopsy frameworks to gather comprehensive insights into the factors leading to maternal mortality. By interviewing bereaved family members and medical examiners, she aims to identify critical areas for improvement in maternal healthcare practices and inform policy changes that can reduce maternal deaths and address disparities in healthcare.
Her dedication to maternal health extends beyond research as she actively engages in community outreach, education, and advocacy. Wendy has begun to present her work at various national and international conferences. Her contributions to the field of maternal health are driven by a profound commitment to closing the gaps in healthcare disparities and improving outcomes for all women.

Dr. Hewlett-Masser, DNP, CNM, IBCLC is a Clinical Educator, Assistant Professor for the University of New Mexico, College of Nursing since 2024. She currently teaches foundational courses in the Doctor of Nursing program in addition to the specific Midwifery specialty track. She practices clinically as a Certified Nurse-Midwife with the University Midwifery Associates in the UNM Department of Obstetrics and Gynecology, specializing in midwifery care for all who seek it. She is an advocate for reproductive justice, recognizing the role of psychological safety in comprehensive reproductive health care. Dr. Hewlett-Masser also advocates for the value of midwifery care in improving maternal child outcomes and increasing access to care. She currently serves Co-president of the New Mexico Affiliate of the American College of Nurse-Midwives and as a member of the New Mexico Department of Health Nurse-Midwifery Advisory Counsel.
Hewlett-Masser earned a Doctor of Nursing Practice and Master of Science in Nursing from Frontier Nursing University. Her doctoral project centered on expanding access to effective perinatal depression care.

Diane Ortega, DNP, CNM is the Co-owner and Administrative Director of Willow Midwife Center for Birth and Wellness AZ with locations in Mesa, Phoenix and Gilbert. The accredited birth centers have been recognized nationally for their excellent outcomes.
She received her Doctorate in Nursing Practice from Frontier Nursing University and additionally holds a post-masters certificate in Integrated Behavioral Health Care-Women’s Health from Cummings Graduate Institute. She helped to spearhead a perinatal behavioral health integration project at Willow Birth Center from 2016-2020 that received international acclaim through publication of outcomes in the International Journal of Integrated. Dr. Ortega and her business partner will be opening the first in the nation inpatient Mother-Baby psychiatric unit for women experiencing severe perinatal mood and anxiety disorders (PMADs).
Dr. Ortega is a member of the Arizona Maternal Mortality Review Committee and the Arizona Maternal Mental Health Advisory Committee. She also serves as the Vice President of the AABC Foundation and President of the AABC Arizona Chapter.

There is no greater honor or joy than guarding and guiding women through the birth journey to motherhood. Jenny is a CNM with Valley Women’s Health in American Fork, Utah. She received her Bachelor of Science in Nursing from California State University at Los Angeles. As a graduate RN, she moved to Colorado, where she worked in critical care for several years, then transferred to teaching as a home dialysis instructor to patients with kidney failure. She met and married her Air Force husband and began her career as a military wife, supporting her family through the necessary frequent moves. After three tours of duty overseas and the birth of her three daughters, Jenny felt called into midwifery and earned her CNM certificate from The Frontier School of Midwifery and Family Nursing, now The Frontier Nursing University. She has practiced as a midwife with the Air Force, the Army, and the Indian Health Service in Alaska. She has experience in home and birth center births and private practice.
Jenny is a member of the American College of Nurse-Midwives and is board-certified by the American Midwifery Certification Board. She is a certified childbirth instructor and trained in lactation support. Jenny Has been certified in Neonatal Resuscitation, Advanced Cardiac Life Support, and Advanced Life Support in Obstetrics. She is credentialed to practice at two hospitals in the area.
Jenny loves the sunshine, gardening, outdoor activities (when not in school), and walking her Bernese Mountain dogs with her now-retired husband. She has been married for 50 years and has raised 3 incredible daughters. She now bears the honorific of Gigi (grandmother glifort) after being gifted with a grandson.

Rebekah Bhansali is a PhD candidate at the Johns Hopkins University School of Nursing with a diverse background in human development and family science, nursing, and nurse-midwifery. She completed her Nurse-Midwifery education at Frontier Nursing University. Rebekah worked as a Certified Nurse Midwife at Allen Midwifery and Family Wellness, a freestanding birth center in the Dallas-Fort Worth Metroplex, providing holistic care throughout adolescence, pregnancy, birth, postpartum, and menopause. Her dissertation research focuses on hypertensive disorders of pregnancy and their long-term cardiovascular risks with considerations of genetic and environmental influences by employing predictive modeling. Rebekah aims to advance precision health and technologies to improve healthcare outcomes and promote equitable lifelong wellbeing for women and birthing individuals.

Amy Holt has served as the Disability Services Coordinator at Frontier Nursing University (FNU) for six years. In this role, she collaborates with faculty, staff, and students to ensure that the needs of students with disabilities are met across all academic areas. Amy serves as an advocate with or on behalf of the students, ensuring they have access to the necessary resources and support.
Prior to her current role at FNU, Amy worked with the Kentucky Department of Vocational Rehabilitation Services in various capacities for nearly eight years. As an American Sign Language (ASL) Interpreter for the D/deaf, DeafBlind, and hard of hearing populations, she adeptly navigated linguistic and cultural variations while thoughtfully applying ethical decision-making skills and best practices. Amy also provided collaborative support for independent living and life skills, advocating tirelessly for individuals’ rights to access within the workplace and beyond. Her efforts aimed at removing barriers and fostering successful outcomes for individuals seeking to gain or maintain competitive integrated employment.
With experience spanning vocational sectors and regions across the Commonwealth of Kentucky, Amy’s expertise in disability services, advocacy, and the success and social justice of individuals with disabilities drives her motivation. As an honored recipient of Frontier Nursing University’s Culture of Caring Award, she remains dedicated to championing inclusivity, access, and empowerment for all.

Dr. Jamal-Eddine’s goal is to create transformative change within healthcare education praxis by developing engaging pedagogic strategies to educate healthcare students about ableism and intersectional identity-based oppression. Her long-term goal is to found an interdisciplinary, applied public-humanities community-engaged healthcare equity center in a university that confronts healthcare inequity, violence, and oppression and promotes intersectional, cross-identity liberation, humanization, and belongingness for all patients, students, and practitioners.

She is an artist, poet, and historian. She uses her art and poetry to bring awareness to maternal health. She provides women’s health care at Planned Parenthood of Southern New England. She currently hosts web discussions Overdue Reckoning on Racism in Nursing. She founded Lucinda’s House, a Black Maternal Health Collective, to promote maternal health equity through community collaboration and programs that provide support and education. Dr. Canty has received funding for her research from the Robert Wood Johnson Foundation.
She has published in various journals, including AJN, American Journal of Nursing, Nursing Inquiry, Journal of Advanced Nursing, Birth, and Nursing Philosophy. Dr. Canty is a contributing editor for the Journal of Midwifery and Women’s Health’s Ask the Midwife Column. Additionally, she is a sought-after nurse scholar in addressing both maternal health equity and anti-racism initiatives. She is a frequent featured speaker virtually and in person at local, regional, national, and international conferences focused on the challenges of reducing disparities in maternal morbidity and mortality.
She is a fellow in the American Academy of Nursing and the American College of Nurse Midwives. She is the 2023 Yale School of Nursing Alumni Association (YSNAA) Distinguished Alumni Award Recipient and the recipient of the 2023 Florence S. Wald Award from the Connecticut Nurses’ Association. She is the 2024 Columbia University School of Nursing 2024 Distinguished Alumni Award for Nursing Practice.

In addition to developing impactful programs, Dr. Meeks plays a pivotal role in advancing equity through her collaborations with health professions associations. Through these collaborations she spearheads efforts to ensure that health science trainees and program leadership receive the support and resources they need to thrive in their respective specialties.
Dr. Meeks is a prolific scholar and widely recognized as a leading expert in this field. Her research findings have been published in leading journals, including the NEJM, Lancet, JAMA, and Academic Medicine, underscoring the significance of her work. Her contributions extend beyond research to the realm of education and advocacy, where she has co-created impactful social media campaigns and podcasts, working tirelessly to promote disabled clinicians and scholars and reduce harmful disability stereotypes in health professions training and STEM.
Within the wide range of accomplishments she holds, Dr. Meeks most valuable role to date is becoming a grandmother. She cites her time with her grandson Charlie as the most rewarding and “bucket filling” moments in her life.

With over 15 years of experience in public health and nursing, Nikia has dedicated herself to advancing reproductive rights and justice, birth justice, and midwifery. Her passion for midwifery shines through in her commitment to diversifying the workforce of midwives and birth workers, especially in the southern United States. As a fervent disruptor of the current healthcare system, Nikia is pioneering new models of care that prioritize midwifery and center the needs of Black and brown communities. Every day, she works Tirelessly to ensure that all individuals have the agency and resources to make informed decisions about their sexual and reproductive health.
At CHOICES Center for Reproductive Health, Nikia serves as the Chief Clinical Officer, spearheading initiatives that have led to the establishment of the first nonprofit comprehensive reproductive health care center, the first Black midwifery fellowship program and the city’s inaugural birth center. Beyond her clinical leadership, Nikia sits on the Board of Directors for both the American College of Nurse Midwives and SisterReach, Tennessee’s foremost Reproductive Justice organization.
All new alumni are automatically welcomed into the FNU Alumni Association. We appreciate the commitment and dedication of our alumni who play an integral role carrying out the FNU mission in everyday practice. Visit our Alumni Association page .
View information including eligibility criteria and ceremony preparation and sign up to participate. August 18, 2023 is the last day to RSVP via the self-registration dashboard (MarchingOrder).
Coming Soon!
New FNU graduates and their guests are invited to join us for a celebration event on the FNU campus following the commencement ceremony, 2:00 p.m. – 6:00 p.m. EST. (will include sign-up Google form link when ready so we can tailor appropriate follow-up)
Local Attractions
Rupp Arena, part of The Lexington Center, is located in a very walkable area of downtown Lexington, KY. The Center is conveniently situated within 10 miles from both I-64 and I-75, and just under 6 miles from Blue Grass Airport. There are numerous hotels and restaurants within easy reach. Below are some links to help you plan your trip:
- Rupp Arena (our event venue)
- VisitLex.com
- KentuckyTourism.com
- Blue Grass Airport
Area Lodging
The following hotels offer special pricing and courtesy holds for FNU commencement guests:
Best Western Parkside Inn – Frankfort
80 Chenault Road, Frankfort, KY 40601 (23.7 miles from the venue, via I-64 E) – 20 rooms per day held for the following 2023 dates: 9/22 & 9/23. Room type(s): Double Queen. Rate: $102 + tax. A credit card is required for a security guarantee. Book by phone: 502.695.6111. You must mention “Frontier Nursing University” to book with this offer . The offer ends on 7/22/2022 or when rooms are filled, whichever comes first.
Holiday Inn Express – Versailles
365 Commerce Drive, Versailles, KY 40383 (12.4 miles from the venue, via US 60) – 10 rooms per day held for the following 2023 dates: 9/22 – 9/23. Room type(s): 5 Single King ($164 + tax) or 5 Double Queen ($174 + tax). A credit card is required for a security guarantee. Refunds are available if requested within the cancellation window. CLICK HERE to book online or call 859-873-5501. When calling, you must mention “Frontier Nursing University” to book with this offer . The offer ends on 8/22/2022 or when rooms are filled, whichever comes first.
Candlewood Suites – Lexington
603 Adcolor Drive, Lexington, KY 40511 (2.0 miles from the venue, via Newtown Pike) – 10 rooms per day held for the following 2023 dates: 9/22 – 9/23. Room type(s): Single Queen Studios Rate: $159 + tax. A credit card is required for a security guarantee. Refunds are available if requested within the cancellation window. CLICK HERE to book online or call 859-967-1940. When calling, you must mention “Frontier Nursing University” to book with this offer . The offer ends on 8/31/2022 or when rooms are filled, whichever comes first.
Homewood Suites by Hilton – Lexington/Hamburg
2033 Bryant Road, Lexington, KY 40509 (6.9 miles from the venue, via Sir Barton Way & Winchester Rd) – 10 rooms per day held for the following 2023 dates: 9/22 & 9/23. Room type(s): King one-bedroom Suite Rate: $175 + tax. A credit card is required for a security guarantee. Refunds are available if requested within the cancellation window. CLICK HERE to book online or call 859-543-0464. When calling, you must mention “Frontier Nursing University” to book with this offer . The offer ends on 8/31/2023 or when rooms are filled, whichever comes first.
Holiday Inn – Lexington/Hamburg
1976 Justice Drive, Lexington, KY 40509 (6.7 miles from the venue, via Sir Barton Way & Winchester Rd) – Rooms held for the following 2023 dates: 9/22 & 9/23. Room type(s): 10 single King/ 10 double Queen; Rate: $149 + tax. A credit card is required for a security guarantee. Refunds are available if requested within the cancellation window. Group Code: FRN CLICK HERE to book online or call 1-888-HOLIDAY. When calling, you must mention “FRN” to book with this offer . The offer ends on 9/8/2023 or when rooms are filled, whichever comes first.
Commencement Ceremony Timeline – Saturday, September 23, 2023:
- 9:00 a.m. EST – doors open at Rupp Arena (ceremony venue)
- 9:00 – 10:30 a.m. EST – Graduate Check-In
- 10:40 – 10:50 a.m. – Lineup for Processional
- 11:00 a.m. EST – Ceremony Processional
- Approx. 1:30 p.m. EST – Ceremony Recessional
- 2:00 – 6:00 p.m. EST – FNU campus celebration event for all new graduates & their guests

The first dancer to be named People Magazine “Women Changing the World,” and named InStyle Magazine Badass 50, Adidas “women reimagining sport,” CBS News “People Making a Difference”, and featured on Good Morning America and NBC Today, Marisa is an award-winning Transformational Movement Artist, Speaker, and Changemaker dedicated to creating a more inclusive just world where we can each feel alive, not just survive.
Marisa’s lived experiences of her body repeatedly not being accepted as a dancer, her Japanese American identity not fitting the box in many spaces, and surviving a stroke that initially paralyzed her from the neck down, eventually led her to create Infinite Flow, an award-winning nonprofit dance company that employs disabled and nondisabled artists with diverse, intersectional identities with a mission to use dance as a catalyst to dismantle biases and promote inclusion.
During the last year, Marisa was diagnosed with two invisible disabilities: PTSD and Autism. The diagnoses brought much clarity to the challenges she’s coped with throughout her life.
Marisa is passionate about transforming forward-thinking businesses through keynotes, performances, and content that inspire inclusivity and move hearts, bodies, and minds, so that their teams become more connected, purpose-driven, and alive. She has brought unique unforgettable keynote presentations and performances to some of the biggest enterprises in the world, including Meta, Apple, Red Bull, NBCUniversal, Deloitte, PayPal, International Monetary Fund, Farmers Insurance, Kaiser Permanente, Porsche, McKinsey & Co, Clifford Chance, amongst other brands. Marisa made history along with wheelchair dancer Piotr Iwanicki by becoming the first dancer to perform at Apple’s Steve Jobs Theater, sharing the stage with Apple CEO Tim Cook.
Since 2015, Marisa has led Infinite Flow to perform at over 160 events, from large global events to local school assemblies & community festivals. Heading the creative & artistic direction, Infinite Flow’s videos have tracked over 100 million views on Facebook alone. During the Covid-19 pandemic, Marisa spearheaded Infinite Flow to turn its in-person elementary school assembly program into a virtual program, launching Scoops of Inclusion, a 47-minute short film celebrating diversity and empowering kids to take an active role in creating a more inclusive world where we each feel we belong.
Marisa is bilingual and bicultural. She completed her BA & MA from Keio University, Tokyo. She is an Honorary Member (Distinguished Artist) of the International Association for Dance Medicine and Science. She is a speaker, thought leader, performing artist, and multi-dimensional creator on the rise, seeking to creatively inspire inclusion, innovation, and transformation through movement, dance, and storytelling.
More on Marisa at MarisaHamamoto.com.

Lucero, Robert J. PhD, MPH, RN, FAAN
Associate Dean for Diversity, Equity, and Inclusion
Professor of Nursing, and Audrienne H. Moseley Endowed Chair in Diversity, Equity and Inclusion
University of California, Los Angeles, School of Nursing
My research program focuses on improving health outcomes of vulnerable populations using innovative health systems and informatics approaches. Two prominent themes of my work are: enhancing the quality of care for hospitalized older adults and improving self-management of chronic health conditions among Hispanic, African-American, and LGBTQ+ populations. My research is distinguished by interdisciplinary team science, which bridges nursing, medicine, psychology, computer science, and engineering, health systems, communities, and other academic institutions.
My research is leading the way to inform infrastructure development for data-driven knowledge generation that serves as a model for organizations across the United States (US) to improve the quality of care for hospitalized older adults. I am leveraging electronic patient, clinical, and administrative data and data science methods to identify valid, modifiable factors that predict hospital-acquired falls (HAF), which affect annually approximately one million US hospitalized patients. Studies I have published show that, in 168 US hospitals, poor nursing care quality was associated with more adverse patient events, including HAF. Using artificial intelligence approaches with electronic health record (EHR) data, I have discovered a set of six new clinical and organizational factors that can predict HAF. These findings were among the most downloaded in 2019, and have widespread implications since hospital patient falls continue to be a significant clinical concern internationally in healthcare systems. My lab also explores the use of registered nurses’ (RNs’) progress notes, or text data on patient observations, to predict HAF. We were the first to publish that RNs’ notes contain information about clinical, environmental, and organizational factors that can predict fall risk. I am Principal Investigator (PI) of a 5-year $2.57 million award from the National Institute on Aging. This cutting-edge health systems project is exploiting the use of text and structured EHR data to validate predictors of HAF and hospital-induced delirium. This study will expand the University of Florida Health EHR research infrastructure for data-driven knowledge generation.
The other cornerstone of my research program is developing health information technology (HIT) to promote chronic disease self-management. I pioneered and published a HIT design approach, known as Consumer-centered Participatory Design (C2 PD). Unlike other design approaches, C2 PD provides public health and community-based organizations, academic researchers, and commercial designers with a theoretically informed approach that engages consumers throughout the development and evaluation of HIT. C2 PD builds on the strengths and resources within a community, promotes a collaborative learning and empowering process, facilitates collaborative partnerships, and incorporates four components of HIT design, namely; user preferences, functions, tasks, and representational requirements, to develop highly usable systems. We introduced this innovative approach and presented our findings to informaticians at the International Medical Informatics Association Nursing Informatics Congress in 2012. We demonstrated that using the C2 PD approach resulted in a highly useful and usable fall prevention self-management system for English- and Spanish-speaking older adults. Since then, multiple investigators of HIT development and systematic review articles have referenced the use of the C2 PD approach. The C2 PD approach has been the basis of my other funded studies, including a $2.8 million National Institute of Nursing Research and $1.0 million Agency for Healthcare Research and Quality award. I have disseminated further wide-ranging use of the C2 PD method, including creating a mobile Health (mHealth) application (app) interface for Hispanic caregivers of persons with dementia to self-manage chronic stress and burden and an mHealth app to support African American caregivers of children with chronic asthma and obesity. The lessons I learned developing the C2 PD approach are represented in a paper I co-authored that focuses on using HIT to engage communities to improve health and reduce health disparities in populations. This is significant to the work I am conducting among people living with HIV. A study I published showed that a large proportion (85.5%) of people living with HIV are interested in using a mHealth app that supports HIV self-management, including functions to identify health services, provide health tips and medication reminders, communicate with healthcare providers, track their mood and emotions, and engage in social networking. My lab is expanding this research with funding from the Health Services and Resources Administration (HRSA) and the Florida Department of Public Health to inform creating and testing a technology-enabled self-management intervention.
I have developed an independent and externally funded health services and informatics research program of over $8.85 million as PI. I publish in high impact journals and researchers and scholars in nursing, health services, and informatics cite my research regularly according to citation analytics (>1024, h-index:14, i10-index:18). Additionally, federal government agencies have recognized my research. I was a standing member of the Agency for Healthcare Research and Quality HIT Research review panel from 2016-2020, and served on multiple NIH Special Emphasis Review Panels. My peers have recognized the impact of my research nationally, and I am disseminating my research program internationally. I am a Fellow of the American Academy of Nursing and the New York Academy of Medicine. In 2019, I received a 3-year UF Term Professorship that acknowledged my academic accomplishments in shaping the UF College of Nursing and the nursing discipline. I am currently the Associate Dean for Diversity, Equity, and Inclusion; Professor of Nursing (with tenure); and, the Adrienne H. Mosely Endowed Chair in Diversity, Equity and Inclusion at the University of California, Los Angeles, School of Nursing.

Born in Orange, California and raised in the beautiful state of Oregon, Rebekka Eshler has had an adventurous life. Being raised by her wonderful grandmother, she learned valuable life lessons earlier than her peers. After graduating high school and a few confusing years in college, Rebekka decided it was time to make a change and decided to join the United States Army and becoming a Fire Support Specialist Paratrooper. Rebekka was stationed all the way up in the last frontier state of Alaska. Even before transitioning, she was embraced by the LGBTQIA’s community.
After leaving the service, Rebekka delayed her transition as she started her professional piloting career at University of Alaska Anchorage. After many nights of deep thought and struggle, Rebekka decided that she loved helping people and redirected her efforts towards a Political Science Degree. She also took biology and chemistry classes because she fell in love with medicine after becoming an Emergency Medical Technician. While at UAA Rebekka’s passion for helping others and leadership got even stronger. She was participated in many different student leadership organization and even became the Student Veterans of America Chapter President at UAA. Rebekka also began working as a volunteer for the Non Governmental Organization Mobile Medics International, that provides medical response to natural disasters and humanitarian crises around the world.
After coming out as a proud trans woman in 2018, Rebekka began reconnecting with her local LGBTQIA community in Anchorage. She began being a major voice for the LGBTQIA Community in her final year of college. From being the first openly transgender SVA UAA Chapter President, to working at the homeless shelter as an EMT, Rebekka wasn’t afraid to speak up and make sure that everyone was receiving equal treatment. After Graduating in 2020, during the pandemic, Rebekka decided it was time to be more active and joined the board of Transgender American Veteran Association as the Director of Strategic Partnerships and Collaborations. In this role she built relationships with other Veteran organizations and LGBTQIA organizations.
Rebekka represented her state as Miss Trans Alaska 2022 and won Miss Congeniality at the national Miss Trans USA 2022 pageant. She is currently serving as the National President of The Transgender American Veteran Association.

Shea Rose has held a variety of titles throughout her career, including singer-songwriter, yogi, style icon, and music curator, to name a few. Her music, influenced by soul, hip-hop, rock, and folk, addresses identity, self-acceptance, and spiritual transformation. Former Boston Globe music critic Steve Morse described her as “that rare artist who can bridge diverse styles such as soul, funk, rock, rap, and jazz — and bring her unique stamp to each.”
Rose is a featured songwriter and vocalist on two Grammy Award-winning jazz albums by legendary drummer Terri Lyne Carrington, The Mosaic Project, and Money Jungle: Provocative in Blue. She has received numerous accolades for her musical abilities, including multiple Boston Music Awards, a SESAC National Performance Activity Award, the Songwriters Hall of Fame’s Abe Olman Scholarship, and, most recently, the Andrea C. Silbert Rising Star Award from the Center for Women & Enterprise for her Embodied Voice & Yoga business.
Rose has independently released three full-length solo projects: Little Warrior Mixtape, Rock’ n Rose EP, and D.T.M.A. (Dance This Mess Around) EP. In 2020, Rose recorded a cover of Sinéad O’Connor’s “Black Boys on Mopeds,” a powerful commentary on police brutality in black communities. The music video was published and promoted by TEDxTalks. Rose has performed in Barbados, Cuba, Jamaica, Italy, Greece, and Romania, as well as at Symphony Hall in Boston, the Blue Note Jazz Club, and SXSW.
Rose is an Assistant Professor at Berklee College of Music. When she’s not on the stage offers Embodied Voice & Yoga coaching and consulting to individuals and organizations. Embodied Voice & Yoga Coaching by Shea Rose is a certified Women and Minority Owned Business whose mission is to empower brown and black women and girls to communicate their highest goals with courage, compassion, and clarity.
For more on Shea Rose visit:
www.shearose.com
www.instagram.com/shearose

Patricia K. Bradley PHD, RN, FAAN is an Associate Professor and the Inaugural Associate Dean of Inclusive Excellence at the Fitzpatrick College of Nursing (FCN) at Villanova University.
Dr. Bradley’s current work focuses on diversity, equity and inclusion and fostering cultural humility in students, faculty, staff, and healthcare providers. Her research and service activities represent her commitment and contribution to ensuring a “voice for the voiceless” and to developing a culture of trust with vulnerable populations who lack access to address their concerns.
Dr. Bradley is a fellow in the American Academy of Nursing. She is the immediate past Chair of the Academy’s Health Equity Expert Panel and a mentor for the Academy’s Jonas Policy Scholars Program’s National Policy Mentoring Council (NPMC).
A graduate of the American Association of Colleges of Nursing’s (AACN) 2022 Diversity Leadership Institute, Dr. Bradley is the chair elect for AACN’s Diversity Equity and Inclusion Leadership Network (DEILN) and a contributor to the Diversity, Equity, and Inclusion Faculty Tool Kit.
At Villanova Dr. Bradley serves as faculty co-advisor for the newly formed Multicultural Student Nurses Organization (MSNO), a service organization developed by students and dedicated to fostering an inclusive environment for historically underrepresented nursing students. Dr. Bradley is also chair of a parallel program, the FCN’s steering committee for Healthy Work Environment Initiatives working with faculty and staff to foster an inclusive environment where all faculty, staff, and students are respected, accepted, and valued.

Dr. Vicki Hines-Martin is a Professor and the Associate Dean, Office of Community Engagement and Diversity Inclusion in the University of Louisville School of Nursing. In addition, she holds a joint appointment as the Director of Community Outreach in the UofL Health Sciences Center Office of Diversity and Inclusion which serves the schools of dentistry, medicine, nursing, and public health. Dr. Hines-Martin is an associate director in the NIEHS funded UofL Center for Integrative Environmental Health Sciences and a Commonwealth Scholar in the Kentucky Commonwealth Institute. She has been a psych-mental health clinical nurse specialist for 36 years. Her area of scholarship includes mental health disparities, culture, social justice/equity, and community engagement.
Dr. Hines-Martin has numerous presentations and publications which include the Routledge Handbook of Global Mental Health Nursing: Evidence, Practice and Empowerment . New York, NY: Routledge/Taylor & Francis Group (Yearwood, E. & Hines-Martin [Eds], 2017). Dr. Hines-Martin has received many awards and recognitions for her work from organizations such as The Global Alliance for Behavioral Health and Social Justice. Dr. Hines-Martin served as the President of the International Society for Psychiatric Mental Health Nursing and is a Fellow in the American Academy of Nursing.

Michelle DeCoux Hampton, RN, PhD, MS is the Director of Academic Nursing and Patient Care Research in the Office of Research Patient Care Services at Stanford Health Care. Dr. Hampton formerly served in a variety of academic roles at Samuel Merritt University (2005-2018) including Professor and Director of the Doctor of Nursing Practice program and at San Jose State University (2018-2022) as Professor and Doctor of Nursing Practice Program Coordinator in the Valley Foundation School of Nursing, as well as Assessment Facilitator and Special Director of Diversity, Equity and Inclusion in the College of Health and Human Sciences.
Her expertise and experience includes psychiatric mental health nursing and research methods for undergraduate, master’s and doctoral students with knowledge of student engagement in various modalities including face-to-face, hybrid, online, and simulation. Her research and service interests are focused on promoting health equity for underserved populations, in part by increasing access to health professional education for members of underrepresented communities, and by educating current students and practicing professionals regarding health equity. As an Advisory Council Member for the Salvation Army, Garden Street Center in Oakland, she spearheaded an initiative to create a certified nursing assistant program within the vocational education program as an entry point to the nursing profession for shelter residents and others in the local community. She also serves as a holistic admissions review consultant for the American Association of Colleges of Nursing providing training for faculty and administrators in US nursing programs. Workshops educate participants in methods to increase diversity within nursing programs that are considering or have already implemented holistic admissions review and/or evaluation.

Kendra M. Barrier. PhD, MSN, RN, CNE
Louisiana State University Health Sciences Center-New Orleans School of Nursing (LSUHSC-NO SON)
Dr. Barrier is an Assistant Professor of Clinical Nursing, serving as the Inaugural Associate Dean for Diversity, Equity, and Inclusion (2021 to present) and the former Assistant Dean for Student Services (2015-2021) at the Louisiana State University Health Sciences Center-New Orleans School of Nursing (LSUHSC-NO). She is also an Associate Faculty for the School of Graduate Studies at LSUHSC-NO, a National League for Nursing (NLN) Certified Nurse Educator, an American Association of Colleges of Nursing (AACN) Diversity Leadership Institute Fellow, and an AACN Elevating Leaders in Academic Nursing (ELAN) Fellow. She a mentor for the third cohort of AACN Diversity Leadership Institute. She provides a strategic vision and leadership by engaging in quality improvement and programmatic development by promoting a culture of inclusive excellence. She is currently piloting the Diversity, Equity, and Inclusion Elements Tool (DEIET), threading DEI through the SON curricula. She is a mentor and coach, and is passionate about the academic success of underrepresentative minority students.
Externally, Dr. Barrier is the President for New Orleans District Nurses Association (2020 to present). An active member several committees and taskforce for the Louisiana State Nurses Association; the Chair of the AACN DEI Leadership Network; and a member of the AACN Organizational Leadership Network (OLN) Steering Committee and Co-Chair of the Communications Committee; a member of the National League for Nursing Education Awards Committee; a member of the American Nurses Association (ANA), a member of the Epsilon Nu Chapter-at-Large of Sigma Theta Tau International (STTI), and a member of the Southeastern Conference (SEC) DEI Collaboration. Dr. Barrier also serves as the Presidential Consultant for the Louisiana Association of Student Nurses. Lastly, she is a member of the New Orleans (LA) Chapter of The Links Incorporated.
Dr. Barrier has presented diversity, equity, and inclusion content, diversity leadership vision, and where DEI fits into Academic Nursing Education locally, regionally, and nationally. She has also been a member of several DEI panel presentations.
She earned her BSN (2000) and MSN (2009), in Nursing Education, from LSUHSC, and received a PhD (2016), in Nursing Education and Administration, from William Carey University.

Jean Edward , PhD, RN, CHPE, is an Associate Professor and Assistant Dean for Diversity, Equity, and Inclusion at the College of Nursing, and Nurse Scientist for UK HealthCare’s Markey Cancer Center.
Dr. Edward’s program of research is focused on promoting equity in healthcare access, affordability, and health outcomes for underserved communities by intervening on the social determinants of health. She utilizes mixed methods and implementation science approaches to design and implement sustainable multi-level interventions that promote equity in access to and affordability of care. She has implemented several nationally funded oncology financial navigation programs to address financial toxicity of cancer experienced by pediatric and adult patients, survivors and caregivers. Dr. Edward has been funded by the National Cancer Institute, Robert Wood Johnson Foundation, American Cancer Society, Kentucky Nurses Association, Sigma Theta Tau International, and the Kentucky Pediatric Cancer Trust Fund. Her work has been published in over 40 peer-reviewed publications and presented at over 70 national, regional, and local conferences. She is the Associate Editor of Clinical Nursing Research and a fellow of the American Association of Colleges of Nursing’s Diversity Leadership Institute.

Heidi Loomis, DM, CRNP, CNM enjoys supporting clinical midwifery and women’s health nurse practitioner students and their preceptors in her role as Regional Clinical Faculty at Frontier Nursing University. She recently completed a Doctorate of Midwifery degree at The Midwifery Institute at Jefferson. Her doctoral research focused on biases that midwifery students across the U.S. experience in their clinical settings – the types and prevalence of bias as well as its impact on midwifery students’ commitment to the completion of their academic programs and to the profession of midwifery. Part of her research also included the emotional responses and behavioral coping mechanisms employed by students in response to bias, whether midwifery students witnessed anyone intervening, and whether or not students reported experiences of bias. For this work, Heidi received the American College of Nurse-Midwives Foundation’s 2022 W. Newton Long Award for the Advancement of Midwifery. Heidi has been interested in culturally respectful care and the growth of midwifery for decades. She has presented to academic, government, non-governmental, and private institutions on topics including anti-racism, privilege, and midwifery. Heidi also enjoyed clinical practice as a family nurse practitioner and certified nurse-midwife for over 30 years in Pennsylvania, Massachusetts, and Connecticut. She is a graduate of Juniata College, Yale School of Nursing, Frontier Nursing University, and The Midwifery Institute at Jefferson, College of Health Professions, Thomas Jefferson University in Philadelphia.

PhD in Human Development
Study in areas of Adult Development and Aging, Child and Adolescent Development, Family Science, and Marriage and Family Therapy.

About Our Program
The doctoral program in Human Development provides a systematic approach to observing, understanding, and analyzing human development across the lifespan, close relationships, and families within their individual, social, and historical contexts. Students complete coursework that includes developmental and systemic theories, qualitative and quantitative research methods and advanced statistical analysis, and opportunities to hone your area of expertise. This program is designed for doctoral students who already hold a master’s degree. For prospective students who do not have a master’s degree, see our MS to PhD in Human Development program.
With a myriad of opportunities to do real-time research through our Child Development Center for Learning and Research (CDCLR) , Family Therapy Center , and the Engagement Center for Creative Aging (ECCA) , our multidisciplinary program provides prepares professionals for careers in academia, social services, health care, government, non-profits, and more.
Virginia Tech Blacksburg Campus
Type of Instruction:
On-Campus In-Person
Adult Development and Aging
Child and Adolescent Development
Family Science
Marriage and Family Therapy
The Department of Human Development and Family Science has four focus areas: Adult Development and Aging (ADA) , Child and Adolescent Development (CAD) , Family Science (FS) , and Marriage and Family Therapy (MFT) . Faculty and students are associated with one or more of these areas reflective of their scholarly interests. The MFT area is the most distinct as students affiliated with this area engage in clinical practice and supervision and complete an internship during their fourth year.
What You'll Study
Required Coursework (17 Credits) +
- HD 5005 HDFS Theories: Individual & Lifespan (3)
- HD 5006 HDFS Theories: Family & Systems (3)
- HD 5114 Adult Development & Aging (3)
- HD 5224 Child Development in the Family Context (3)
- HD 5324 Marriage & Family Relationships (3)
- HD 6004 Professional Development Seminar (2)
Methods & Statistics Requirements (21 Credits)
- HD 5514 Research Methods (3)
- HD 5974 Research Methods Lab (1)
- HD 5524 Qualitative Research (3)
- HD 5714 Regression (3)
- HD 5974 Regression Lab (1)
- HD 6514 Advanced Research Methods (3)
- HD 6524 Advanced Research Methods Lab (1)
- Additional Methods Course (3)
- Additional Methods Course (3)
Elective Coursework+
Students pick at least 2 electives; examples include
- HD 5224 Sexual Health & Human Rights (3)
- HD 5334 Perspectives of Human Sexuality (3)
- HD 5254 Social Epidemiology and Health Inequities (3)
- HD 5714 Mixed Methods (3)
- HD 5644 Program Development and Evaluation (3)
- HD 5654 Grant Writing and Administration (3)
Research and Dissertation+
- HD 7994 Research and Dissertation (30)
- HD 5964 Research Team (4)
Why choose this program?
- The doctoral program focuses on theory and research training.
- Our small program enables students to get individualized attention from our award-winning and research-active faculty.
- All of our doctoral students receive funding through research and/or teaching assistantships, dependent on satisfactory performance and progress to degree.
- Faculty actively publish and present with students, and our graduate students are also encouraged to lead research projects and publish in scholarly journals.
- Our department provides students with a plethora of research opportunities, including experimental and observational research in laboratory settings, field research in the surrounding communities, and secondary data analysis.
- Numerous rewarding career opportunities are available for doctoral graduates in Human Development, including teaching, research, administration, and extension service. A wide range of career options exist outside the academy as well, such as program development and evaluation, policy analysis and advocacy work, and administration and supervision in private and public human services agencies.
Admissions and Tuition
Admissions requirements.
- A bachelor's degree and master’s degrees with minimum GPA 3.0 (4 Scale)
- TOEFL/IELTS (For all non-U.S. citizens or non-U.S. permanent residents)
- Transcripts (official copy must be sent after students receive an offer of admission)
- Three letters of recommendation
- Letter of Interest and CV
- Writing Sample
Application Deadlines
Domestic and International
- December 1st for next Fall semester start
Funding Opportunities
We are currently able to provide assistantship funding to all graduate students who make timely and satisfactory progress. All Ph.D. students that maintain full-time status and maintain a 3.0 GPA will be offered an assistantship (20 hours of work per week). Assistantships may include research obligations, teaching undergraduate level courses, or other administrative tasks. Students on assistantships receive a monthly stipend, tuition waivers/remission, and health benefits.
Related Programs
366 Wallace Hall 295 West Campus Drive Blacksburg, VA 24061 [email protected]
Marty Wyatt , Graduate Staff Coordinator 540-231-4794 [email protected]
Erika L. Grafsky , Director of Graduate Studies [email protected]
Share Options
- Share to Facebook
- Share to Linkedin
UVA Researchers Develop New Coatings to Boost Turbine Engine Efficiency
Innovative Materials Could Lead to Cleaner Energy and Lower Costs
A University of Virginia-led research team has developed new protective coatings that allow turbine engines to run at higher temperatures before components begin to fail.
“Hotter engines are more efficient,” said Elizabeth J. Opila , professor and chair of the Department of Materials Science and Engineering at UVA and a lead researcher on the project.
Turbine engines are known for aircraft propulsion, but stationary turbines have many industrial uses, including power generation. They burn fuel to rotate turbine blades, converting mechanical energy to electricity.
“You get more work output per heat input at higher temperatures,” Opila said. “The potential benefits drive interest in coatings that act as a barrier against the reactive gases produced by combustion at these high temperatures that can damage turbine blades.”
Efficiency translates to less fuel consumption and reduced emissions and operating costs — which helps account for why the U.S. Department of Energy’s ARPA-E ULTIMATE program funded the team’s work. They published their findings in the October print issue of Scripta Materialia.
Limits of Today’s High-Temperature Materials

Two primary material systems are used in the hot section of turbine engines today:
- Coated nickel-based superalloys can tolerate up to about 2,200°F — well short of the DOE’s goal of nearly 3,300°F.
- Ceramic composites use several coating layers to protect against degradation from oxidation, a chemical reaction that occurs with exposure to air and moisture. However, these systems are limited by the melting temperature of one layer, silicon, which melts at 2,577°F.
The UVA-led team focused on another material option called refractory metal alloys. Refractory metals were studied extensively in the 1960s. While durable and heat-resistant, they were abandoned due to poor oxidation resistance.
To protect the alloy, the researchers experimented with rare earth oxides — chemical compounds that naturally possess strong protective properties — to come up with one do-it-all coating.
“By combining multiple rare earth oxides, tailoring properties to better protect the underlying substrate can be achieved with just a single layer,” said Kristyn Ardrey, a Ph.D. alumna of Opila’s lab and first author of the paper. “This allowed us to achieve better performance without complex multi-layer coatings.”
A Multidisciplinary Team Approach
Opila’s lab created and tested new combinations of rare earth elements, such as yttrium, erbium and ytterbium. To predict the best combinations and improve performance, they worked with UVA associate professors Bi-Cheng Zhou and Prasanna Balachandran , whose labs specialize in computer simulations and machine learning, a form of artificial intelligence.
The team applied the coatings to alloys using two standard manufacturing methods. One technique heats the material to a molten state before spraying on the surface. The other is applied as a liquid mixture that dries and hardens. The researchers tested and compared how well each method performed under extreme heat and reactive conditions, such as exposure to high-temperature steam.
By combining multiple rare earth oxides, tailoring properties to better protect the underlying substrate can be achieved with just a single layer.
They also partnered with UVA Professor Patrick Hopkin s' ExSiTE Lab, which specializes in using lasers to measure heat resistance and material strength.
“This was a collaborative effort,” Opila said. “Using machine learning and computational methods allowed us to explore a huge range of possible material combinations, and Patrick’s lab was key to understanding the physical characteristics of the materials we developed.”
More Work To Be Done
As one of the first research groups to experiment with multicomponent rare earth oxides, the team knows more testing and refinement are needed. Using computer simulations will help them continue improving the coatings and analyze the best ways to apply them.
But their results represent an important step forward in turbine engine technology — and that’s good for everyone.
“Reducing fuel consumption and emissions while improving engine performance is not only good for industries like energy and aviation,” Opila said. “It also means a cleaner environment and lower costs for everyday consumers.“
Publication
“ Opportunities for novel refractory alloy thermal/environmental barrier coatings using multicomponent rare earth oxides ” was first published online June 4, 2024.
Additional UVA contributors include Mackenzie J. Ridley, Kang Wang, William Riffe, Mukil Ayyasamy and Mahboobe Jassas, representing the departments of Materials Science and Engineering, Mechanical and Aerospace Engineering, and Physics. Kevin Reuwer, Giavanna Angelo and Carolina Tallon of the Department of Materials Science and Engineering at Virginia Tech and Kevin Childrey and Jonathan Laurer of the Commonwealth Center for Advanced Manufacturing also were collaborators.
The Office of Naval Research provided additional funding.
Diverse Expertise
Want to know more about the researchers in this story and how UVA Engineering is advancing high-temperature materials technology through multi-disciplinary approaches? Follow the links below to visit our faculty lab websites.

COMMENTS
UVA's PhD in nursing program is focused on research, and the curriculum includes courses in qualitative, quantitative, and historical research. Over the course of the program, all PhD students submit a research proposal for peer review, and many submit proposals to the NIHNR's annual service awards competition.
Virginia's top-ranked nursing programs $ 4.7M. in scholarships and aid in 2024. 3 % In the top 3% of U.S. graduate nursing programs. Let us help you find your fit. Loading... RSVP FOR AN UPCOMING ADMISSIONS ZOOM. PhD Zoom Info Session on Oct 23 at 5:30pm. ... by the Rector and Visitors of the University of Virginia.
of U.S. graduate nursing programs. $4.74M. in scholarships distributed in 2024 to 67% grad students. flexible programs. that meet you where you are in your personal and professional journey. Our graduate programs are designed for working nurses like you to achieve your career goals: whether that is actualizing the many roles of an advanced ...
MSN - Master of Science in Nursing. Virginia's top-ranked nursing programs and ranked among the top 3% of American graduate nursing programs, we offer graduate programs for nurses at every professional stage. As healthcare grows increasingly complex, the necessity for advanced practice nurses to coordinate and deliver stellar care has never ...
Associate Professor of Nursing. Director, School of Nursing Continuing Education. Graduate Nursing Programs. CMNEB 2113. (434) 924-0115. [email protected]. Barbara Reyna, PhD, RN, NNP-BC. Associate Professor of Nursing. Department Chair of Graduate Nursing Programs.
The Ultimate Advanced Practice Nurse. The Doctor of Nursing Practice (DNP) empowers nurses who want to practice at the highest clinical level: in addition to making treatment decisions, ordering tests, and prescribing medications, they also lead people and teams and improve systems and safety, occupying roles in academia, as nurse ...
Doctor of Philosophy in Nursing Suggested Plan of Study: Full time. * Each School of Nursing course is identified by a 4-digit academic credit nomenclature: Please Visit the Graduate Record for the official program requirements for the Doctor of Philosophy in Nursing. The information contained on this website is for informational purposes only.
All applicants for the PhD possess a BSN. Many also possess an MSN, and nurses with other graduate degrees (MPH, MBA, MS in Health Administration, etc.) are also encouraged to apply. If you are applying to the UVA School of Nursing PhD program, you should be aware that the following tenured and tenure-track faculty are eligible to accept students:
The University of Virginia Records contain information about academic resources, policies and procedures, college and department programs, and undergraduate and graduate course offerings of the University. ... Graduate Record 2024-2025 Nursing, Ph.D. Print-Friendly Page (opens a new window) ...
graduate program (and awarded a grade of "" or higher) toward the 72-hour doctoral requirement. In any case, at least 18 graded course credits applied toward the degree must have been earned at the University of Virginia. If nine or more transfer credits are awarded, the student's date of graduation will be accelerated by one term.
List of University of Virginia School of Nursing graduate programs by size and degree. Browse popular PhD programs at University of Virginia School of Nursing. Find on-campus and online graduate programs at University of Virginia School of Nursing.
The University of Virginia graduate student experience couples the resources of a large state university, with the mentorship of a personalized program. With more than a hundred advanced degrees to choose from, our graduate students take advantage of one-on-one attention with world-class faculty, state-of-the art facilities and the highest ...
Graduate Admission. Thomas Jefferson believed that learning was a lifelong pursuit. From the arts and sciences to law and business, UVA offers some of the nation's premier graduate programs. Darden School of Business. Frank Batten School of Leadership and Public Policy.
Purpose. The DNP program at the University of Virginia School of Nursing prepares graduates to drive the highest level of advanced nursing practice. Through direct or indirect care roles, our graduates are prepared to lead system level initiatives that provide high quality care while optimizing population health and improving outcomes.
For international students who are not U.S. citizens, UVA and the School of Nursing do not have funds available for scholarships or loans. As a result, international applicants applying to the School's undergraduate and graduate programs (BSN, RN to BSN, CNL, RN to CNL, MSN, post-master's, and DNP) must be prepared to finance the entire cost of ...
Programme Structure Curriculum: With a DNP, you'll earn all the personal, financial, and professional benefits a doctoral degree brings; as a UVA School of Nursing graduate, you'll also reap the rewards and connections a degree from Virginia's top-ranked nursing program offers.
All admitted students to the PhD program are eligible to be awarded four years of scholarship to cover tuition, insurance, and fees, in exchange for serving as a GTA for 10 hours per week. The University of Virginia offers a fully funded PhD in Nursing. All applicants for the Ph.D. possess a BSN. Many also possess an MSN and other degrees.
The University of Virginia Records contain information about academic resources, policies and procedures, college and department programs, and undergraduate and graduate course offerings of the University. ... Graduate Record 2023-2024 Nursing, Ph.D. Print-Friendly Page (opens a new window) ...
The online terminal degree readies nurses for careers in education and research to advance the profession of nursing. PhD Programs. Doctor of Philosophy (Ph.D.) ... University of Virginia. PhD Programs. Doctor of Philosophy in Nursing (PhD) Campus; 225 Jeanette Lancaster Way Charlottesville, VA 22903-3388 (434) 924-0141.
Dr. Maddox received her B.S. in biology from Virginia Union University, Richmond, and her Ph.D. in physiology from Georgetown University. ... She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. ... 502.695.6111. You must mention "Frontier Nursing University" to ...
The doctoral program in Human Development provides a systematic approach to observing, understanding, and analyzing human development across the lifespan, close relationships, and families within their individual, social, and historical contexts. Students complete coursework that includes ...
A University of Virginia-led research team has developed new protective coatings that allow turbine engines to run at higher temperatures before components begin to fail. "Hotter engines are more efficient," said Elizabeth J. Opila , professor and chair of the Department of Materials Science and Engineering at UVA and a lead researcher on ...