

Nursing Report Writing Guide for Nursing Students

Report writing is essential in any profession, and since nursing is also considered a profession, one must record their work after shift completion. A good nurse report should contain the following details: patient history, diagnoses, vitals labs, medications, and more. Nurses must show accountability for their work and duty to the patient by writing a proper report. An excellent report ensures continuity of care. You are likely to compromise the health and safety of a patient if you don't fill out all the important details. According to studies by John Hopkins University , medical error is the third leading cause of death in the US. For this reason, it's important to know how to write one correctly.
This guide will show you how to write the perfect nursing report.
What is a Nursing Report?
Also known as an end shift report, or a nurse brain, a nursing report is a compilation of all important patient details written by a nurse at the end of a shift. It highlights the record of a patient's medical background, situation, treatment, and care plan. This report helps in facilitating handoffs . For instance, a nurse coming in for their day shift would get a report from the nurse finishing their night shift.
Writing a good nursing report ensures a seamless handover to the incoming nurse who may not be familiar with the patient and their needs.
These reports also go with a patient being transferred to another hospital or department, for instance, if the patient is being transferred from the ICU to the recovery room.
Please keep in mind that nursing reports should be made promptly if they are to serve their purpose.
What to Include in a Nursing Report
A nursing report shows the patient's current medical status. When writing one, there are essential things that you should include. These things are,
Basic information:
- Date of admission
- The patients doctor(s)
- Medical history (all preexisting conditions or any infectious diseases)
- Code status
- Power of attorney
- Advanced directives, for instance, DNR (Do Not Resuscitate)
Current patient health details
- Vital signs (blood pressure, oxygen levels, temperature
- Neuroinflammation
- Musculoskeletal data
- Dietary restrictions
- Wounds or pain points
- The patient took medication
- IV access and the types of fluids
Ongoing patient care information
- Medication dosage and when they should be administered
- Lab results or any pending lab work
- Other tests needed
- How long will the patient stay in the hospital, or when should they be discharged
- Any future procedures that require preparations
- Additional information about requests by the patient
These details are essential; providing them to the incoming nurse helps them keep track of the patient.
Other types of information you will likely see on a nurse report include:
- Patients' preferences, e.g., food, room temperature
- Routine reminders (does the patient require supervised walks)
- Any triggers
- Emergency contact details
- Language barrier (does the patient need a translator)
Steps to Writing a Good Nursing Report
You need to organize the process well to develop an efficient report that won't raise any issues. You must also write it on time to provide the patient with safe and high-quality service.
Follow these steps to fill out your nursing report:
Understand the Purpose of the Report
Before completing the report, you must understand its importance and the application area. This way, you will intelligently communicate the information. Remember that reports not supported by facts are considered useless and worthless.
Use the SOAP Method
The SOAP method is the order in which the medical note is written, and it follows the following plan: Subjective, Objective, Assessment, and Plan. It's vital to arrange your information in the following plan for a professional view.
Nurses use the SOAP method in their reports to make writing easy for others to understand.
Fill in the Basic Information
Begin by filling the template with essential information like the patient's age, sex, date, and time. Include your knowledge as well.
Note that you should not review any routine care procedures now.
Collect Subjective Evidence
Once you have filled in the basic information, collect subjective details from the patient. This information is limited to the knowledge and perspective of the patient or family member accompanying them. Pay attention when you are given this information, especially what they report about their symptoms and past diseases.
Some of the information you will collect about the patient include the pain points and level, the purpose of their visit, and any other concern they might have about their health.
Also, provide any other healthcare problems and diagnoses. Make sure you compare this information to the patient's age.
When collecting this information, you must remain calm and show some level of compassion. You should also be patient, especially when dealing with difficult patients or family members.
Filling in the Objective Information
After collecting all the subjective information from the patient and family members, you should gather objective information. Objective information is that which supports subjective details. Including this information is necessary because it will lead to the patient's diagnosis. Objective information includes the patient's blood work, vitals, observable symptoms, and any tests ordered by the attending doctor.
Also, include any observations you've made about the patients' health and responses. Ensure you stress any recent changes but don't include critical information about the patient's behavior.
Write Down Your Assessment
Assessment involves sorting and analyzing the information provided to learn more and make an informed decision about the patient's health, care plan, and current decision-making.
Jot down the conclusions based on the objective information collected and the conclusion made by the primary care physician. Additionally, include the prescribed medication and how the patient responds to it. Also, note any changes the patient has shown since being administered (are their symptoms improving or worse?)
A lack of assessment can pose a risk to the patient, so you must include this section.
Related: How to write a nursing diagnosis (NDx)
Write a Care Plan
A care plan section outlines the needs and wants of the patients and any interventions you make to meet them. For instance, if the patient needs a lab or imaging test, include it in this section. Also, ask how the patient is responding to the care plan. If, for example, you advise the patient to return to the hospital for a checkup and they fail to show up, include it in the report.
You should write this section well because it will help show the plan's effectiveness. It also acts as evidence that care was given to the patient.
Write Down the Interventions
Interventions are actions you take to help the patient achieve their expected outcomes. This section can include different types of information, including physical treatments, emotional support, and education given to the patients about their ailments, medication, and current or future treatment. Also, include details such as when you gave the patient their medication.
Tips on How to Write a Nursing Report
When filling out a nursing report, you must remember that you are not just writing; you are also communicating. Another nurse or doctor will use your report to decide on the patient's care plan.
As such, nursing reports should be easy to read. Use the following tips to help you write a perfect report.
Ask for Help
If you don't understand how to write the report or which direction to take when asking for information, ask for help. It's not shameful or embarrassing to confess that you don't understand how to fill some sections. Most hospitals and doctors use the SOAP method to write nursing reports, but some offer templates. If you are working in a new hospital or clinic, ask for help from your supervisor. You can also delegate the task to an online nursing/medical report writing service like ours.
Be Objective
Remaining objective as you collect and fill out the nursing report is important.
To be objective is to be unbiased; when you are, it means feelings do not lead you. When collecting data, use your senses: hearing, sight, smell, and touch, to assess the patient. You will collect this type of information during a physical examination.
When you remain objective when collecting this data, you will keep the progress report accurate and precise.
Use Active Voice
Instead of passive voice, use active voice because it is direct. Active voice involves writing sentences with the subject performing the action. Using an active voice in your report will bring clarity by stressing to the reader who is taking action.
Active : I administered 500mg of paracetamol to the patient.
Passive : 500mg of paracetamol was administered to the patient.
The problem with passive voice is that it leaves important details out.
Only Include Important Information
Don't write unnecessary information. You have to find a balance between being detailed and concise. Being concise involves providing as much information with as few words as possible. Rambling around in your report will not serve any purpose but only create confusion. Also, you don't want to include unnecessary information that will make it harder to follow the report. The best way to ensure your report is okay is to use the provided nursing report template.
Use Good Communication
No matter how casual you are with your colleagues or supervisor, it would help if you left this during breaks or outside working hours. You must be professional when writing a nursing report or any other kind of report. You must approach patients to understand their concerns, fears, symptoms, etc. This means that your listening, verbal, and nonverbal verbal skills should always reflect a level of professionalism.
Related Readings:
- How to use the SBAR communication tool
- Making a nursing concept map
- Steps for writing a QI nursing report
- Steps for writing a perfect EBP paper
Add the Information Later
While speaking to the patients and gathering the information, it is important to use an outline and fill in the details later. Finishing consultation ensures you give your all to the patient and what they say. You should also attend to one patient and write the report before proceeding to the next patient because it will help you remember the notes more clearly. However, if you can't finish the notes before attending to the next patient, you should write the most important details first.
Check Other Nurse's Report
Over time, each nurse will develop their voice in the reports. Reading how other nurses, exceptionally experienced ones, have written their reports will help you develop your skill and see improvement areas. Getting inspired by sample nursing or medical reports is a great way to write the best one.
Be Clear on the Priorities
Since a nursing report is given at shift changes, you must be as straightforward as possible. For instance, if you discover a pain relief measure that is effective on the patient during your shift, including the information will ensure the next nurse continues with the same pain relief measure.
Also, if there are procedures that should be conducted as soon as possible, include them in the order they should be done.
Make Your Writing Legible
Please take note that a nursing report aims at ensuring continuity of care. If your text cannot be skimmed, it defeats its purpose. All the information in the report is sensitive, and if you make a mistake, it will have severe consequences for the patient.
When writing the report, write every word, phrase, and sentence well. Also, use the right medical terminology. This way, you will show not only authority but also credibility.
Avoid Late Entries
Late entries are any information absent in the original entry recorded after writing the original report. The problem with late entries is that they tend to introduce inaccuracies. If you must introduce a late entry, ensure you follow the hospital's or clinic's policy on going about it.
Remember that constant late entries will portray you in a bad light.
Write Down All Consulted Physicians
If you consulted any physician while caring for the patient, include it in your report. For instance, if you consulted a gynecologist or oncologist concerning any symptoms the patient was experiencing, mention it in the report. Write them down, starting with their names, titles, times, responses, and resulting actions.
Follow the Facility's Policy on Abbreviations
Even though the use of the medical abbreviation is not a new thing, care should be taken when using them. It's easy to make mistakes by inappropriately using abbreviations. If you have to use abbreviations, ensure they are approved by the facility you work for.
Avoid Hearsay and Personal Opinion
Hearsay or personal statements will carry less weight on the paper. Only write details that are supported by facts. If you have to write personal opinions, use quotations to show them.
Also, be honest in your report, especially when you've made a mistake. Honesty won't always protect you against consequences but will preserve your reputation and moral code.
Common Errors in Nursing Report
Now that you know how to write your report, here are some common errors to avoid.
Omitting Meditation
Knowing the kind of medication that a patient is taking or those that they are allergic to is critical to their care. Always specify every medication they take, the dosage amount, and how the patient reacts to them. In the same manner, knowing that a patient is allergic to penicillin or other antibiotics is the difference between treating them with the right medication or causing more health problems.
Leaving Some Sections Blank
Omitting drugs is wrong, but leaving important sections blank is worse. The incoming nurse expects to find a well-written report to help them continue caring for the patient. If you haven't done this, how will they go on? Blank spaces create ambiguity. Did you leave it blank because treatments weren't administered, or you forgot to write the treatment?
Spending Time on Unnecessary Information
There is such a thing as too much unnecessary information in nursing reports. The aim of these reports is to document the crucial facts that can help with patient care. There are things that you shouldn't put in your report because they are irrelevant, or the next nurse can quickly look up and understand.
Writing unnecessary information will take too much of your time, which you could use to write the next patient's report. Such information includes:
- Non-essential comorbidities. There are patients with a lot of them, which would take time to talk or write about them.
- Every drug the patient is on. Again some patients can have a long list of medications that is not necessary to list. So stick to the important ones.
- Specific labs- if needed, the next patient will have all this information with them.
Using your judgment when writing this is essential to avoid wasting time on unnecessary details. When in doubt, you can always consult your supervisor.
Before you click Exit, ....
Report writing is a crucial part of the nursing routine. A nurse's reports help registered nurses stay organized and capture all the important patient details like diagnosis, vital signs, allergies, pain management plans, and more. Providing this information ensures the next nurse does not risk the patient's life by making mistakes such as failing to prescribe the right medication. The above tips should help you write the perfect nurse report if assigned one as a nursing student.
Related Articles
- How to do a head-to-toe assessment
- Steps for writing a nursing dissertation or thesis
- Overcoming nursing school challenges
- How to do a critical appraisal of nursing scholarly articles
- How to write a windshield survey report
You can also trust our legit/reliable nursing writing services to get help. We write 100% original, well-researched, cited, and polished nursing reports for nursing students. Do not let poor grades bother you. Use your time in cursing school to have fun and get deserved rest.
Struggling with

Hardest Nursing Classes and How to Pass Them Well
Nursing Information Systems: Pros and Cons, Types, and Examples

Epidemiology Research Essay: A Guide with Steps, Insights, & Tips
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.

How to Give an Effective Nursing Report: A Comprehensive Guide

Giving a nursing report is a critical task that ensures continuity of care, patient safety, and effective communication between healthcare professionals. Whether you're a seasoned nurse or just starting in the field, mastering the art of giving a thorough and concise nursing report is essential. This guide will walk you through the best practices for delivering a high-quality nursing report, ensuring that you provide the necessary information clearly and effectively.
1. Understanding the Purpose of a Nursing Report
The primary goal of a nursing report is to transfer essential information about a patient's condition, treatment, and progress from one nurse to another during shift changes. A well-delivered report ensures that the incoming nurse is fully informed and can continue providing appropriate care without missing critical details.

2. Preparing for the Nursing Report
Preparation is key to giving a smooth and comprehensive report. Here’s how to prepare:
- Review Patient Records: Before starting your report, review the patient’s chart, medication list, and any recent lab results or imaging studies. Ensure that all documentation is up-to-date.
- Organize Your Thoughts: Jot down notes on each patient to ensure you cover all necessary points. Use a standardized format, such as SBAR (Situation, Background, Assessment, Recommendation), to keep the report organized.
- Update the Care Plan: Make sure that any changes in the care plan are documented and will be included in your report.
3. Using the SBAR Format
The SBAR method is a widely accepted framework for delivering nursing reports. It helps structure the information in a way that’s easy to follow and understand. Here’s how to use SBAR:
- Situation: Start with the patient’s name, room number, and the reason for their admission or current status. Briefly describe the situation that requires attention.
- Background: Provide relevant medical history, including diagnoses, allergies, and any recent procedures or treatments.
- Assessment: Share your clinical assessment of the patient, including vital signs, lab results, and any notable changes in condition.
- Recommendation: Offer your recommendations for ongoing care, including any follow-up actions, pending tests, or medications that need to be administered.
Free Report Sheet Downloads:
4. Key Elements to Include in Your Report
To ensure your report is comprehensive, make sure to cover these essential elements:
- Patient Identification: Start with the patient’s full name, age, gender, and room number.
- Diagnosis and Admission Information: Mention the primary diagnosis, any secondary diagnoses, and the date of admission.
- Vital Signs and Assessments: Include the latest vital signs, pain assessment, and any other relevant findings (e.g., neurological status, respiratory function).
- Current Treatments: Discuss the medications administered, IV fluids, oxygen therapy, wound care, and other ongoing treatments.
- Recent Changes: Highlight any changes in the patient’s condition, treatments, or lab results during your shift.
- Pending Orders and Tests: Inform the incoming nurse of any tests that are pending or treatments that need to be carried out.
- Special Considerations: Mention any patient-specific details, such as allergies, isolation precautions, or dietary restrictions.
5. Effective Communication Tips
The way you deliver your report is just as important as the content. Here are some communication tips to enhance your report:
- Be Clear and Concise: Avoid unnecessary details or jargon. Stick to the facts and keep your report focused.
- Use Active Listening: Encourage the incoming nurse to ask questions or seek clarification if needed. Active listening ensures both parties are on the same page.
- Maintain Professionalism: Stay calm and professional, even if the situation is stressful. Your demeanor can influence how the report is received.
6. Common Pitfalls to Avoid
To ensure your report is as effective as possible, avoid these common mistakes:
- Being Disorganized: A disorganized report can lead to confusion and missed information. Stick to a structured format like SBAR to keep your report on track.
- Overloading with Information: While it’s important to be thorough, avoid overwhelming the incoming nurse with too much information. Focus on what’s most relevant to patient care.
- Neglecting to Follow Up: If there are critical issues that require follow-up, make sure to emphasize these points in your report.
7. The Importance of Continuity of Care
A well-delivered nursing report is crucial for ensuring continuity of care. It allows the incoming nurse to pick up where you left off, minimizing the risk of errors and enhancing patient outcomes. By mastering the art of giving a nursing report, you contribute to a safer and more efficient healthcare environment.
Giving a nursing report is an essential skill that directly impacts patient care and safety. By preparing adequately, using a structured format like SBAR, and focusing on clear and concise communication, you can ensure that your reports are both comprehensive and effective. Practice these tips and continuously refine your reporting skills to become a more competent and confident nurse.
Enhancing Nursing Education Through Curriculum Mapping
Nursing educators are continually challenged to bridge the gap between classroom learning and clinical practice, and curriculum mapping has become a powerful tool to streamline this transition, allowing educators to align course objectives with essential skills and competencies. Paired with electronic clinical tracking systems (ECTS) like NurseTasks, curriculum mapping not
Preparing for Accreditation: How Electronic Clinical Tracking Simplifies Compliance for Nursing Programs
Accreditation is one of the most critical aspects of running a nursing program. It ensures that the education provided meets national standards, preparing students for professional practice and helping schools maintain their reputation. However, managing the accreditation process can be overwhelming, particularly when it comes to documenting clinical hours, competencies,
How Nursing Educators Can Help Improve Their Students' Time Management Skills
Time management is an essential skill for nursing students, as it directly impacts their ability to succeed both academically and clinically. Effective time management not only helps students meet their educational goals, but also prepares them for the fast-paced, high-stakes environment of healthcare. Nursing educators play a critical role in
Leveraging Data and Analytics in Nursing Education
Data and analytics continue to enhance outcomes and refine teaching practices in nursing education. By utilizing these technologies, educators can gain deep insights into student performance, tailor instruction to meet individual needs, and ultimately produce more competent and confident nursing professionals. 🏫Learn more about NurseTasks for educators and institutions. The
- Paragraph Generator
- Cover Letter
- Authorization Letter
- Application Letter
- Letter of Intent
- Letter of Recommendation
- Business Plan
- Incident Report
- Reference Letter
- Minutes of Meeting
- Letter of Resignation
- Excuse Letter
- Research Proposal
- Job Application
- Acknowledgement
- Employment Letter
- Promissory Note
- Business Proposal
- Statement of Purpose
- Offer Letter
- Deed of Sale
- Letter of Interest
- Power of Attorney
- Solicitation Letter
20+ SAMPLE Nursing Report in PDF

Nursing Report
20+ sample nursing report, what is a nursing report, what are the information needed in a nursing report, what is the difference between a nursing report and medical report, purpose of a nursing report, steps in writing a nursing report, what to expect after writing a report, what do i need to tell the patient and the patient’s family, do you dread writing a nurse report.
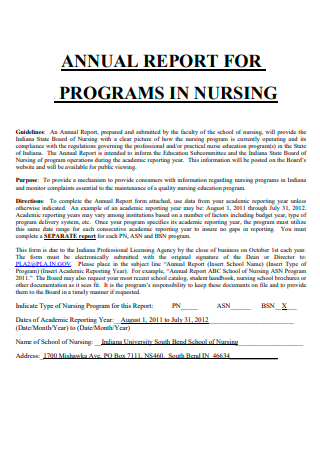
Nursing Annual Report For Programs

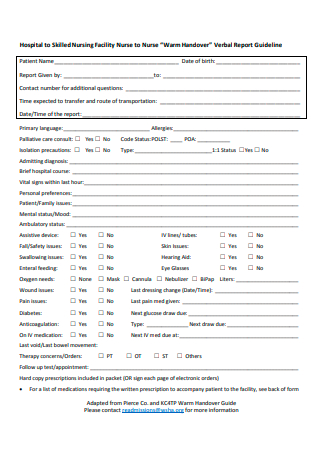
Continuous Skilled Nursing Care Report

Nursing Home Staffing Summary Report

Nursing Educational Programs Report
Basic Nursing Report

Annual Nursing Education Program Report

Annual Non-Public School Nursing Report Form
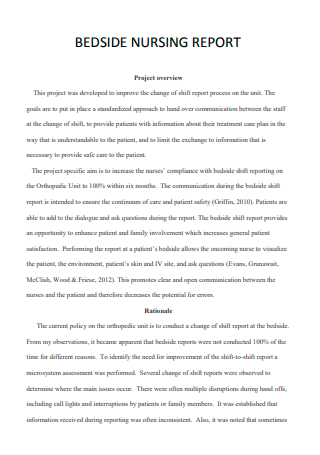
Bedside Nursing Report
Nursing Report Example

Board of Nursing Annual Report

Nursing Report in PDF
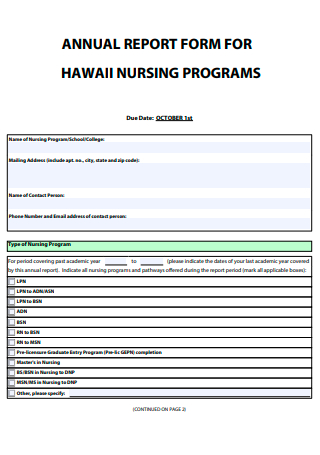
Nursing Programs Annual Report Form

Nursing Salary Research Report
Nursing Excellence Report
Printable Nursing Report

Simple Nursing Report
Nursing Homes Licensing Report

Nursing Services Report
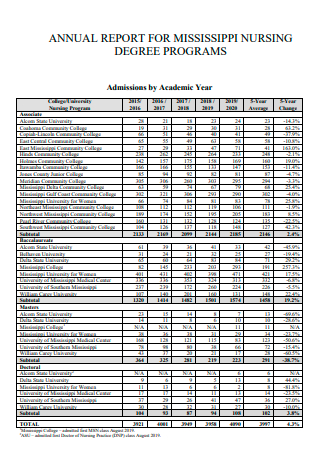
Nursing Degree Programs Annual Report
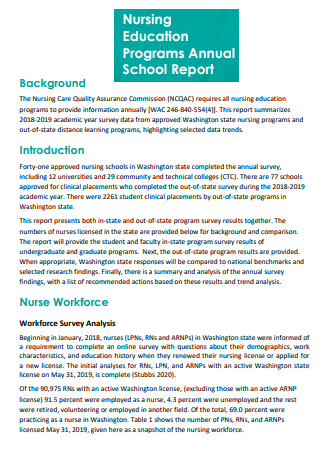
Nursing Education Programs Annual School Report
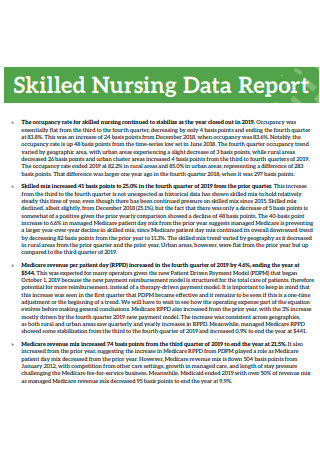
Skilled Nursing Data Report
Step 1: use clinical reasoning and judgment, step 2: meet and document the statements, step 3: input the necessary information, step 4: do not include subjective information, step 5: do not document report in patient’s medical record, step 6: verify the nursing report form and affix signature and data, share this post on your network, you may also like these articles, joining report.
A Joining Report is a formal document submitted by a new employee on their first day at work. It confirms their arrival, position, and date of joining, helping HR…
Sports Report

A sports report is a detailed summary of sporting events, outcomes, and analysis. It is designed to provide readers with the latest scores, statistics, and insights about teams, players,…
browse by categories
- Questionnaire
- Description
- Reconciliation
- Certificate
- Spreadsheet
Information
- privacy policy
- Terms & Conditions

IMAGES
VIDEO
COMMENTS
Giving a nursing report is an essential skill that directly impacts patient care and safety. By preparing adequately, using a structured format like SBAR, and focusing on clear and concise communication, you can ensure that …
A nursing report is a document that nursing students and nursing employees write on a daily basis. It consists of the recorded status of a patient under their care. Why is it …
Well-written nursing progress notes provide detailed information about a patient’s progress for nurses and other healthcare team members to track changes in the patient’s status.
20+ SAMPLE Nursing Report. What Is a Nursing Report? What Are the Information Needed in a Nursing Report? What Is the Difference Between a Nursing Report and Medical Report? Purpose of a Nursing Report. Steps in …
Nursing notes are a narrative written summary of a given nursing care encounter. This might include a description of a nursing visit, a specific care event, or a summary of care. A nurse’s note is a form of charting that describes …
A nursing narrative note is a type of nursing documentation used to provide clear, detailed information about the patient. A narrative note is written in paragraph form and tells a story, if you will, about the patient, the care he is …